Blog
- Ritalin's Impact on the Developing Brain
- By Jason von Stietz, M.A.
- July 31, 2017
-
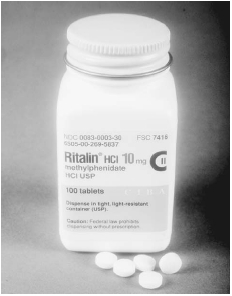
Getty Images Does medication taken to treat ADHD in children have a long-term impact on the brain? Researchers in the Netherlands examined the impact of methylphenidate, or ritalin, on the developing brain. The researchers used magnetic resonance spectroscopy scans to determine that methylphenidate use before the age of 23 related to altered levels of GABA, an inhibitory neurotransmitter, in the medial frontal cortex. The study was discussed in a recent article in Medical Xpress:
“The prevalence of ADHD has increased rapidly over the last few years,” said Michelle M. Solleveld of the University of Amsterdam, the study’s corresponding author. “With this, prescription rates of methylphenidate, also known as Ritalin, are increasing as well. The safety and efficacy of methylphenidate treatment in adults has been studied thoroughly. However, methylphenidate treatment for ADHD is actually more common in children, and no studies so far have investigated the possible long-term effects of methylphenidate on the developing brain.”
“Animal studies show that when animals were treated with methylphenidate during their childhood, persisting effects in the brain remained present well into adulthood,” Solleveld told PsyPost. “This alarmed me, as this hasn’t been studied in humans, but psychiatrists are increasingly prescribing methylphenidate to children to acutely decrease their symptoms of ADHD. I, together with the rest of the research group, therefore wanted to investigate this in humans in order to gain more knowledge about these possible persisting effects.”
The researchers used Magnetic Resonance Spectroscopy scans to examine GABA levels in the medial prefrontal cortex of 44 male ADHD patients. They found evidence that methylphenidate use by children produced long-lasting alterations in GABA neurotransmission in this region of the brain.
“This study focuses on one specific neurotransmitter system: the GABA system,” Solleveld explained. “We report that there are lasting changes in this neurotransmitter system when ADHD patients are treated before the age of 23 years old, i.e. during brain development.”
“This was not the case when treatment was started after the age of 23, when the brain was matured. These results indicate that treatment with methylphenidate in childhood does alter this specific neurotransmitter system in the brain in a long-lasting manner.”
Patients who were treated for the first time with stimulants as children showed significantly lower GABA levels in the medial prefrontal cortex, compared to those who started treatment as adults. A dose of methylphenidate also produced a significant increase in GABA levels in patients treated in childhood, but not in patients treated in adulthood.
But more research is needed to strengthen the preliminary findings and understand its implications.
“We now know that there are lasting alterations in the GABA system in the brain after treatment during brain development,” Solleveld told PsyPost. “We do however not know yet whether and how this is expressed in for example a person’s behavior, performance on psychological tests or other personal characteristics.
“Additionally, we only focused on a specific neurotransmitter system, in only 1 voxel (‘cube’ of 2.5×3.5×2.5cm) in the brain, namely in the medial prefrontal cortex. Future studies should address other systems in the brain or focus on behavioral aspects of possible lasting effects of methylphenidate treatment during brain development.”
“This study is part of a larger project, called the ‘effects of Psychotropic drugs on Developing brain (ePOD),'” Solleveld added. “This study consists of a randomized clinical trial part, in which 50 children and 49 adults were treated for 4 months with either methylphenidate or placebo, and a cross-sectional study. We are currently analyzing all the data of both the cross sectional study and the clinical trial, and expect to report more on this topic in the near future. Please find another publication of our group here: http://jamanetwork.com/journals/jamapsychiatry/fullarticle/2538518.”
The study, “Age-dependent, lasting effects of methylphenidate on the GABAergic system of ADHD patients“, was also co-authored by Anouk Schrantee, Nicolaas A.J. Puts, Liesbeth Reneman, and Paul J. Lucassen.
Read the original article Here
- Comments (0)
- Poverty and Malnutrition's Affect on the Brain
- By Jason von Stietz, M.A.
- July 25, 2017
-

Nature Researchers in Dhaka Bangladesh are studying the link between stunted growth related to impoverished conditions and brain development. About 40% of children in Dhaka suffer from stunted growth by the age of two and findings from magnetic resonance imaging scans show these children to have significantly lower smaller volumes of grey matter than their healthy counterparts. The study was discussed in a recent article in Nature:
In the late 1960s, a team of researchers began doling out a nutritional supplement to families with young children in rural Guatemala. They were testing the assumption that providing enough protein in the first few years of life would reduce the incidence of stunted growth.
It did. Children who got supplements grew 1 to 2 centimetres taller than those in a control group. But the benefits didn't stop there. The children who received added nutrition went on to score higher on reading and knowledge tests as adolescents, and when researchers returned in the early 2000s, women who had received the supplements in the first three years of life completed more years of schooling and men had higher incomes.
“Had there not been these follow-ups, this study probably would have been largely forgotten,” says Reynaldo Martorell, a specialist in maternal and child nutrition at Emory University in Atlanta, Georgia, who led the follow-up studies. Instead, he says, the findings made financial institutions such as the World Bank think of early nutritional interventions as long-term investments in human health.
Since the Guatemalan research, studies around the world — in Brazil, Peru, Jamaica, the Philippines, Kenya and Zimbabwe — have all associated poor or stunted growth in young children with lower cognitive test scores and worse school achievement2.
A picture slowly emerged that being too short early in life is a sign of adverse conditions — such as poor diet and regular bouts of diarrhoeal disease — and a predictor for intellectual deficits and mortality. But not all stunted growth, which affects an estimated 160 million children worldwide, is connected with these bad outcomes. Now, researchers are trying to untangle the links between growth and neurological development. Is bad nutrition alone the culprit? What about emotional neglect, infectious disease or other challenges?
Shahria Hafiz Kakon is at the front line trying to answer these questions in the slums of Dhaka, Bangladesh, where about 40% of children have stunted growth by the age of two. As a medical officer at the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) in Dhaka, she is leading the first-ever brain-imaging study of children with stunted growth. “It is a very new idea in Bangladesh to do brain-imaging studies,” says Kakon.
The research is innovative in other respects, too. Funded by the Bill & Melinda Gates Foundation in Seattle, Washington, it is one of the first studies to look at how the brains of babies and toddlers in the developing world respond to adversity. And it promises to provide important baseline information about early childhood development and cognitive performance.
Kakon and her colleagues have run magnetic resonance imaging (MRI) tests on two- and three-month-old children, and identified brain regions that are smaller in children with stunted growth than in others. They are also using other tests, such as electroencephalography (EEG).
“Brain imaging could potentially be really helpful” as a way to see what is going on in the brains of these young children, says Benjamin Crookston, a health scientist at Brigham Young University in Provo, Utah, who led studies in Peru and other low-income countries that reported a link between poor growth and cognitive setbacks.
The long shadow of stunting
In 2006, the World Health Organization (WHO) reported an extensive study to measure the heights and weights of children between birth and the age of five in Brazil, Ghana, India, Norway, Oman and the United States3. The results showed that healthy, well-fed children the world over follow a very similar growth trajectory, and it established benchmarks for atypical growth. Stunted growth, the WHO decided, is defined as two standard deviations below the median height for a particular age. Such a difference can seem subtle. At 6 months old, a girl would be considered to have stunted growth if she was 61 centimetres long, even though that is less than 5 centimetres short of the median.
The benchmarks helped to raise awareness about stunting. In many countries, more than 30% of children under five meet the definition; in Bangladesh, India, Guatemala and Nigeria, over 40% do. In 2012, growing consensus about the effects of stunting motivated the WHO to pledge to reduce the number of children under five with stunted growth by 40% by 2025.
Even as officials started to take action, researchers realized there were serious gaps in protocols to identify the problems related to stunting. Many studies of brain development relied on tests of memory, speech and other cognitive functions that are ill-suited to very young children. “Babies do not have much of a behavioural repertoire,” says Michael Georgieff, a paediatrician and child psychologist at the University of Minnesota in Minneapolis. And if parents and doctors have to wait until children are in school to notice any differences, it will probably be too late to intervene.
That's where Kakon's work fits in. At 1.63 metres, she is not tall by Western standards, but at the small apartment-building-turned-clinic in Dhaka where she works, she towers over most of her female colleagues. On a recent morning she was with a mother who had phoned her in the middle of the night: the woman's son had a fever. Before examining the boy, Kakon asked his mother how the family was and how he was doing at school, as she usually does. Many parents call Kakon apa — a Bengali word for big sister.
About five years ago, the Gates Foundation became interested in tracking brain development in young children living with adversity, especially stunted growth and poor nutrition. The foundation had been studying children's responses to vaccines at Kakon's clinic. The high rate of stunting, along with the team's strong bonds with participants, clinched the deal.
To get the study off the ground, the foundation connected the Dhaka team with Charles Nelson, a paediatric neuroscientist at Boston Children's Hospital and Harvard Medical School in Massachusetts. He had expertise in brain imaging — and in childhood adversity. In 2000, he began a study tracking the brain development of children who had grown up in harsh Romanian orphanages. Although fed and sheltered, the children had almost no stimulation, social contact or emotional support. Many have experienced long-term cognitive problems.
Nelson's work revealed that the orphans' brains bear marks of neglect. MRIs showed that by the age of eight, they had smaller regions of grey and white matter associated with attention and language than did children raised by their biological families4. Some children who had moved from the orphanages into foster homes as toddlers were spared some of the deficits.
The children in the Dhaka study have a completely different upbringing. They are surrounded by sights, sounds and extended families who often all live together in tight quarters. It is the “opposite of kids lying in a crib, staring at a white ceiling all day”, says Nelson.
But the Bangladeshi children do deal with inadequate nutrition and sanitation. And researchers hadn't explored the impacts of such conditions on cerebral development. There are brain-imaging studies of children growing up in poverty — which, like stunting, could be a proxy for inadequate nutrition6. But these have mostly focused on high-income areas, such as the United States, Europe and Australia. No matter how poor the children there are, most have some nutritious foods, clean water and plumbing, says Nelson. Those in the Dhaka slums live and play around open canals of sewage. “There are many more kids like the kids in Dhaka around the world,” he says. “And we knew nothing about them from a brain level.”
The marks of adversity
By early 2015, Nelson's team and the Bangladeshi researchers had transformed the humble Dhaka clinic into a state-of-the-art lab. For their EEG equipment, they had to find a room with no wires in the walls and without air-conditioning units, both of which could interfere with the device's ability to detect activity in the brain.
The researchers also set up a room for functional near-infrared spectroscopy (fNIRS), in which children wear a headband of sensors that measure blood flow in the brain. The technique gives information about brain activity similar to that from functional MRI, but does not require a large machine and the children do not have to remain motionless. fNIRS has been used in infants since the late 1990s, and is now gaining traction in low-income settings
The researchers are also performing MRIs, at a hospital near the clinic. So far, they have scanned 12 babies aged 2 to 3 months with stunted growth. Similar to the Romanian orphans and the children growing up in poverty in developed countries, these children have had smaller volumes of grey matter than a group of 20 non-stunted babies. It is “remarkably bad”, Nelson says, to see these differences at such a young age. It's hard to tell which regions are affected in such young children, but having less grey matter was associated with worse scores on language and visual-memory tests at six months old.
Some 130 children in the Dhaka study had fNIRS tests at 36 months old, and the researchers saw distinct patterns of brain activity in those with stunting and other adversity. The shorter the children were, the more brain activity they had in response to images and sounds of non-social stimuli, such as trucks. Taller children responded more to social stimuli, such as women's faces. This could suggest delays in the process by which brain regions become specialized for certain tasks, Nelson says.
EEG detected stronger electrical activity among children with stunted growth, along with a range of brainwaves that reflect problem solving and communication between brain regions. That was a surprise to the researchers, because studies in orphans and poor children have generally found dampened activity7. The discrepancy could be related to the different types of adversity that children in Dhaka face, including food insecurity, infections and mothers with high rates of depression.
Nelson's team is trying to parse out which forms of adversity seem to be most responsible for the differences in brain activity among the Dhaka children. The enhanced electrical signals in EEG tests are strongly linked to increases in inflammatory markers in the blood, which probably reflect greater exposure to gut pathogens.
If this holds up as more children are tested, it could point to the importance of improving sanitation and reducing gastrointestinal infections. Or maternal depression could turn out to be strongly linked to brain development, in which case helping mothers could be just as crucial as making sure their babies have good nutrition. “We don't know the answers yet,” says Nelson.
The participants tested at 36 months are now around 5 years old, and the team is getting ready to take some follow-up measurements. These will give an idea of whether or not the children have continued on the same brain-development trajectory, Nelson says. The researchers will also give the five year olds IQ and school-readiness tests to gauge whether the earlier measurements were predictive of school performance.
A better baseline
One of the challenges of such studies is that researchers are still trying to work out what normal brain development looks like. A few years before the Dhaka study began, a team of British and Gambian researchers geared up to do EEG and fNIRS testing on children in rural Gambia during the first two years of life. They were also funded by the Gates Foundation.
Similar to the Dhaka study, the researchers are looking at how brain development is related to a range of measures, including nutrition and parent–child interaction. But along the way, they are trying to define a standard trajectory of brain function for children.
There is a big push at the Gates Foundation and the US National Institutes of Health to nail down that picture of normal brain development, says Daniel Marks, a paediatric neuroscientist at Oregon Health & Science University in Portland, and a consultant for the foundation. “It is just a reflection of the urgency of the problem,” he says.
One of the hopes for the Dhaka study, and the motivation for funding it, is that it will reveal distinct patterns in babies' brains that are predictive of poor outcomes later in life and could be used to see whether interventions are working, says Jeff Murray, a deputy director of discovery and translational sciences at the Gates Foundation.
Any such intervention will probably have to include nutrition, says Martorell. He and his colleagues are doing yet another follow-up study of the Guatemalan villagers to see whether those who got protein supplements before the age of 7 have lower rates of heart disease and diabetes 40 years later. But nutrition alone is unlikely to be enough — either to prevent stunting or to promote normal cognitive development, Martorell says. So far, the most successful nutritional interventions have helped to overcome about one-third of the typical height deficit. And such programmes can be very expensive; in the Guatemalan study, for example, the researchers ran special centres to provide supplements.
Nevertheless, researchers are striving to improve interventions. A group involved in the vaccine study in Bangladesh is planning to test supplements in pregnant women in the hope of boosting babies' birth weight and keeping their growth on track in the crucial first two years of life. Tahmeed Ahmed, senior director of nutrition and clinical services at the diarrhoeal-disease research centre, is planning a trial of foods such as bananas and chickpeas, to try to promote the growth of good gut bacteria in Bangladeshi children aged 12 to 18 months. A healthy bacterial community could make the gut less vulnerable to infections that interfere with nutrient absorption and that ramp up inflammation in the body.
Ultimately, it's not about whether children have stunted growth or even what their brains look like. It's about what their lives are like as they grow older. Studies such as the one in Dhaka strive to help determine whether interventions are working sooner rather than later. “If you have to wait until kids are 25 years old to see whether they are employed,” Murray says, “it could take you 25 years to do every study.”
Read the original article Here
- Comments (0)
- fMRI Predicts And Monitors Change in PTSD Symptoms Following Psychotherapy
- By Jason von Stietz, M.A.
- July 19, 2017
-

Researchers from Stanford University School of Medicine investigated the use of brain imaging to predict the effectiveness of psychotherapy and measure changes in the brain following treatment. The researchers utilized functional magnetic resonance imaging (fMRI) with 66 participants diagnosed with post-traumatic stress disorder (PTSD), who were undergoing exposure therapy. The findings were discussed in a recent article in MedicalXpress:
PTSD is a serious mental disorder that can develop after a dangerous or traumatic event. Patients experience recurring memories of the event; avoid situations, people or thoughts that remind them of the event; and experience altered mood and thinking patterns. Nearly 7 percent of people in the United States will suffer from PTSD at some point in their lifetime, according to the National Institute of Mental Health.
Prolonged exposure therapy for PTSD consists of a series of sessions and homework assignments that lead patients to gradually approach trauma-related memories and situations. Patients begin by imagining scenarios that trigger their PTSD symptoms—such as a crowded park. Then, they work up to deliberately putting themselves in those scenarios. Revisiting traumatic experiences in this manner can, over time, allow the brain to slowly reduce its response to emotional triggers. However, not all PTSD patients derive benefit from the treatment, and about a third drop out of the arduous process, according to Etkin, who is also an investigator at the Veterans Affairs Palo Alto Health Care System. About two-thirds of patients receiving prolonged exposure therapy see a 50 percent reduction in symptoms, and 40 percent of them achieve remission, he said.
To learn how prolonged exposure therapy works in the brain, the studies used functional magnetic resonance imaging to measure the brain activity of 66 patients diagnosed with PTSD as they completed five tasks tapping a variety of emotional and cognitive functions. During these tasks, patients would view, for example, images of faces or scenes—like happy, neutral or scared faces or a scene depicting an event meant to induce negative emotions, such as an argument or physical violence—and either respond to questions about the images or try to control their response to the image's content.
After the initial brain imaging, about half the participants underwent nine to 12 sessions of prolonged exposure therapy; the remainder did not. At the end of the trial, all participants went through the same emotional response and regulation tests while researchers measured brain activity.
A step closer to personalized treatment
One of the studies focused on whether brain activity levels before treatment could help scientists predict which participants would respond well to prolonged exposure therapy. The researchers measured how active certain brain regions were during the five tasks and looked for associations with reduced symptoms post-treatment.
Prior to receiving prolonged exposure therapy, patients with both lower activity in the amygdala and higher activity in various regions of the frontal lobe while viewing faces with fearful expressions showed a larger reduction in PTSD symptoms following therapy. Fonzo refers to the amygdala, seated deep within a primitive region of the brain, as the brain's alarm system, as it plays an important role in fear and other emotional responses. The frontal lobe is the outer layer of the human brain in the area behind the forehead; it plays a role in complex functions such as behavior, personality and decision-making.
The researchers also found that patients with greater activation in a deep region of the frontal lobe when ignoring the distracting effects of conflicting emotional information—such as a picture of a scared face with the word "happy" written across it—responded better to exposure therapy.
"The better able the brain is at deploying attention- and emotion-controlling processes, the better you respond to treatment," said Fonzo.
Using this information about how the brain responds in emotional regulation and processing tasks, the team was able to predict how effective prolonged exposure therapy treatment would be for patients with up to 95.5 percent accuracy. This kind of screening approach, perhaps using the less expensive and more widely available electroencephalogram rather than fMRI, could help doctors determine the best course of PTSD therapy in the future, the researchers said.
"Not only could it provide a ray of hope for patients who would benefit from prolonged exposure to make it through the tough course," said Goodkind, "it means patients who wouldn't derive a benefit wouldn't have to start the treatment."
Therapy changes the brain
In the second study, the researchers found that prolonged exposure therapy led to lasting changes in participants' brains that were associated with improvement in PTSD symptoms. About four weeks after therapy ended, fMRI showed elevated activity in the front-most region of the frontal lobe, an area called the frontopolar cortex. This region is the most recently evolved part of the human brain. It balances internal and external attention and helps coordinate multiple processes in the brain simultaneously, said Fonzo, as would occur when multitasking and remembering future to-do list items.
The role the frontopolar cortex plays in prolonged exposure therapy was surprising, Fonzo said, because much of the scientific attention on emotional processes in PTSD has centered on the amygdala.
Specifically, the changes the researchers observed in frontopolar cortex activity occurred when participants were instructed to regulate their emotional response to an image of a negative or stressful scenario, such as one depicting an argument. The researchers also noted changes in frontopolar cortex activity in these participants during a resting, nonfocused state. The changes in frontopolar cortex activity indicate a shift in frontopolar function following therapy, according to the authors.
The post-therapy brain changes also included increased connectivity between the frontopolar cortex and deeper brain regions closer to emotional processing areas. The authors wrote that psychotherapy may train the frontopolar cortex "to better evoke or amplify attention toward an internal regulatory process that mediates successful emotion regulation."
The degree to which activity in the frontopolar cortex increased following therapy was associated with the degree of improvement in PTSD symptoms and emotional well-being.
Exploring use of transcranial magnetic stimulation
To confirm whether the frontopolar cortex controls important brain regions for emotional processing, the team used a noninvasive method of stimulating brain activity called transcranial magnetic stimulation, or TMS, to activate the frontopolar cortex in healthy people. They simultaneously recorded brain activity with fMRI and confirmed that the frontopolar cortex modulated downstream activity in lower cortical regions closer to emotion-processing parts of the brain.
They also explored whether TMS might help PTSD patients respond to prolonged exposure treatment. Building off their findings that greater frontal lobe and less amygdala activation predicts better treatment outcome, the researchers activated a region of the frontal cortex with TMS probes while imaging the brain. They found that doing so inhibited activity in the amygdala, and the degree to which that happened also predicted the degree to which a patient's symptoms improved. In the future, stimulating this region may help increase patients' responsiveness to psychotherapy, they said. Indeed, some small-scale studies in which therapeutic TMS was used daily on the same region of the frontal cortex, without the addition of psychotherapy, have already shown promising results.
"These findings put a place marker in our understanding of psychotherapy writ large. We can really put psychiatric disorders on the map in terms of hard science and help fight the stigma that surrounds these illnesses and their treatment," said Etkin. "Within the field of PTSD, it gives a concrete sense of hope for people undergoing treatment and starts laying the groundwork for new treatments based on understanding brain circuitry."
Read the original article Here
- Comments (0)


 Subscribe to our Feed via RSS
Subscribe to our Feed via RSS