Blog
- Tool Making And How the Brain Might Have Evolved
- By Jason von Stietz
- April 30, 2015
-
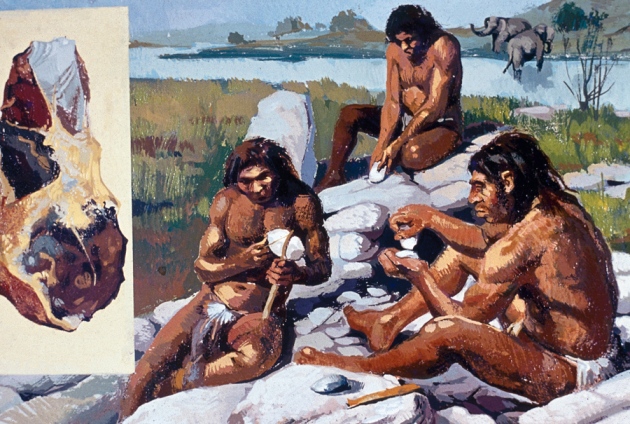
Photo Credit: Getty Images Did the advent of tool making drive the evolution of the human brain? Researchers disagree. However, a recent study using MRI scans offers insight into the debate. The study was discussed in a recent article of Scientific American:
For many decades, scientists have tried to understand the past by doing as our forebears did. One important endeavor in what is called experimental archaeology involves moderns crafting Stone Age tools by chipping away at rocks. Why toil at whittling rocks by hand using other rocks when machine tools are readily available?
One reason is to get at the question of what role toolmaking may have played in brain evolution, given the demands this task places on both mental faculties and motor skills. Toolmaking’s contribution to human evolution is controversial, though. Some theorists suggest that Paleolithic tool manufacture has little to with neural development, others hold that it is a driving force for our swollen frontal lobes.
The advent of the brain scanner has opened up the possibility of finding out who is right. I talked to Dietrich Stout, a professor of anthropology at Emory University about a recent paper in PLOS One that looked at the demands on brainpower that toolmaking placed on our Paleolithic ancestors from 500,000 to 2.6 million years ago. Also check out this video.
1. Why is there a need to do experiments to link toolmaking to brain evolution?
Skulls (endocasts) provide important but limited evidence and can only tell us about whole brain size and shape, and maybe a little about surface features. If we are interested in how brain functions change over the course of evolution, we have to get at them indirectly through evidence of behavior, such as tool-making.
2. Describe your experiment reported recently in PLOS One.
We trained subjects for two years to make stone tools. It’s harder than you think! It can take hundreds of hours of dedicated practice to learn how to make a nice handaxe. It is even more difficult to figure out without some coaching.
Subjects in our studies actually did learn to make tools, though, and we also collected MRI scans at the beginning middle and end. In the scanner, we asked subjects to answer questions about tools we showed them—questions that dealt with decisions about how to shape a tool. By asking different questions, we distinguished basic perceptual-motor skill (understanding how rock breaks) from strategic planning abilities (choosing the right places to hit the rock to achieve a goal). We studied two different tool-making technologies – the simple Oldowan which is the earliest known technique from 2.6 million years ago and the more sophisticated Late Acheulean handaxe technology of about 500, 000 years ago.
3. What did you find? Did it in some way provide hints of the evolution of higher mental functions?
We found that strategizing about how to make a tool was associated with activation of prefrontal cortex associated with the “executive” control of cognition—that is, holding information in mind while manipulating it. More specifically the pattern of activity suggested “mental time travel,” a complex cognitive ability to run mental simulations by projecting into the future or past. Think for example of planning out a home improvement project by mentally running through the steps and trying to identify problems before they happen. We found that this was necessary for the handaxe technology but not the earlier Oldowan, meaning that these artifacts can help us trace the timing and context for the emergence of this important human ability. It even suggests that the demands of learning to make stone tools may have been part of what drove the evolution of this capacity.
4. How important was toolmaking as a driver of evolution? Is it possible that it had something to do with the development of language?
Well, we don’t know for sure but our research has provided evidence suggesting it may have been quite an important driver. It’s not in this paper but my other publications have looked quite a bit at the link with language. There is increasingly strong evidence that an underlying mental ability to construct and understand complex, hierarchically structured sequences is important for both language and tool-making, so that selection on tool-making ability could have provided a “preadapted” base from which language later emerged.
5. Can you describe your Learning to Be Human Project (or the Language of Technology not sure which) project and what it’s trying to achieve?
This just-published study came from the Learning to be Human project, which is now over. The goal was to train modern subjects to make stone tools and observe all aspects of the learning process so we could better understand the challenges faced by our Paleolithic ancestors, and extract more information from the enigmatic stone artifacts that make up our “Stone Age” archaeological record.
Read the original article Here
- Comments (0)
- Variability in Brain Activity Related to Better Cognitive Performance in Older Adults
- By Jason von Stietz
- April 27, 2015
-

Photo Credit: Getty Images As baby boomers continue to age, interest in cognitive performance in older adults will continue to increase. Recent research has identified a marker of cognitive health in the aging brain. Researchers found variability in brain activity to relate to cognitive performance. The study was discussed in a recent article in NeuroScientistNews:
Researchers in the Beckman Institute’s Lifelong Brain and Cognition Lab investigate the brain for differences in cognitive performance among healthy aging individuals.
As we age, the physical make up of our brains changes. This includes changes in neural processing in grey matter, but also in the deterioration of structural connections in the brain, which allow communication between distinct brain regions, so the brain is able to work as a well-wired network system.
Researchers at the Lifelong Brain and Cognition Lab at the Beckman Institute for Advanced Science and Technology at the University of Illinois have utilized the magnetic resonance imaging (MRI) facilities available in Beckman's Biomedical Imaging Center to measure the moment-to-moment variability in brain activity, more specifically in the blood oxygenation level-dependent (BOLD) signal.
In recent years, researchers have observed that this variability in the BOLD signal in the function of certain brain regions may be a good thing, linked to younger age and better cognitive performance. Greater variability may reflect more flexible or adaptive information processing.
However, the association between BOLD variability and structural brain connectivity is not well understood. Also unknown is the association between brain signal variability and cognitive performance on various tasks such as memory, reasoning, speed, vocabulary, and semantic knowledge. Beckman researchers collected functional and structural MRI and looked at cognitive performance in 91 elderly, non-demented adults. They found that older adults who had greater variability in neural activity in specific brain regions performed better on fluid ability and memory tasks, and also had better quality of structural white matter connections in the brain.
Their paper, "White matter integrity supports BOLD signal variability and cognitive performance in the aging brain," is published in PLOS ONE.
"Our study is important as it explores the relationships between moment-to-moment variability in spontaneous brain activity and broadly defined cognitive performance in older adults," said Agnieszka Burzynska, postdoctoral researcher in the Lifelong Brain and Cognition Lab and author of the study. "We think that greater variability in brain function in certain regions allows better processing of information, especially during highly demanding memory and reasoning tasks, which require someone to remember information, form associations, or perform abstract mental operations. We believe that variability in the brain activity reflects the dynamic use of different brain networks. In the aging research, there are mixed findings on whether aging is associated with increased or decreased amplitude of neural activity, and looking into variability of the signal gives us a new type of information on how the aging brain works."
Read the orginal article Here
- Comments (1)
- Memories Might Be Stored in Cell Body
- By Jason von Stietz
- April 17, 2015
-
Photo Credit: Getty Images Where do human memories exist? Past research has suggested that memories take the form of new synaptic connections. However, recent research from UCLA has indicated that memories might be stored inside the cell body. The study was discussed in a recent article in Scientific American:
As intangible as they may seem, memories have a firm biological basis. According to textbook neuroscience, they form when neighboring brain cells send chemical communications across the synapses, or junctions, that connect them. Each time a memory is recalled, the connection is reactivated and strengthened. The idea that synapses store memories has dominated neuroscience for more than a century, but a new study by scientists at the University of California, Los Angeles, may fundamentally upend it: instead memories may resideinside brain cells. If supported, the work could have major implications for the treatment of post-traumatic stress disorder (PTSD), a condition marked by painfully vivid and intrusive memories.
More than a decade ago scientists began investigating the drug propranolol for the treatment of PTSD. Propranolol was thought to prevent memories from forming by blocking production of proteins required for long-term storage. Unfortunately, the research quickly hit a snag. Unless administered immediately after the traumatic event, the treatment was ineffective. Lately researchers have been crafting a work-around: evidence suggests that when someone recalls a memory, the reactivated connection is not only strengthened but becomes temporarily susceptible to change, a process called memory reconsolidation. Administering propranolol (and perhaps also therapy, electrical stimulation and certain other drugs) during this window can enable scientists to block reconsolidation, wiping out the synapse on the spot.
The possibility of purging recollections caught the eye of David Glanzman, a neurobiologist at U.C.L.A., who set out to study the process in Aplysia, a sluglike mollusk commonly used in neuroscience research. Glanzman and his team zappedAplysia with mild electric shocks, creating a memory of the event expressed as new synapses in the brain. The scientists then transferred neurons from the mollusk into a petri dish and chemically triggered the memory of the shocks in them, quickly followed by a dose of propranolol.
Initially the drug appeared to confirm earlier research by wiping out the synaptic connection. But when cells were exposed to a reminder of the shocks, the memory came back at full strength within 48 hours. “It was totally reinstated,” Glanzman says. “That implies to me that the memory wasn't stored in the synapse.” The results were recently published in the online open-access journal eLife.
If memory is not located in the synapse, then where is it? When the neuroscientists took a closer look at the brain cells, they found that even when the synapse was erased, molecular and chemical changes persisted after the initial firing within the cell itself. The engram, or memory trace, could be preserved by these permanent changes. Alternatively, it could be encoded in modifications to the cell's DNA that alter how particular genes are expressed. Glanzman and others favor this reasoning.
Eric R. Kandel, a neuroscientist at Columbia University and recipient of the 2000 Nobel Prize in Physiology or Medicine for his work on memory, cautions that the study's results were observed in the first 48 hours after treatment, a time when consolidation is still sensitive.
Though preliminary, the results suggest that for people with PTSD, pill popping will most likely not eliminate painful memories. “If you had asked me two years ago if you could treat PTSD with medication blockade, I would have said yes, but now I don't think so,” Glanzman says. On the bright side, he adds, the idea that memories persist deep within brain cells offers new hope for another disorder tied to memory: Alzheimer's.
Read the original article Here
- Comments (0)
- One Journalist's Adventures in Transcranial Direct-Current Stimulation
- By Jason von Stietz
- April 10, 2015
-
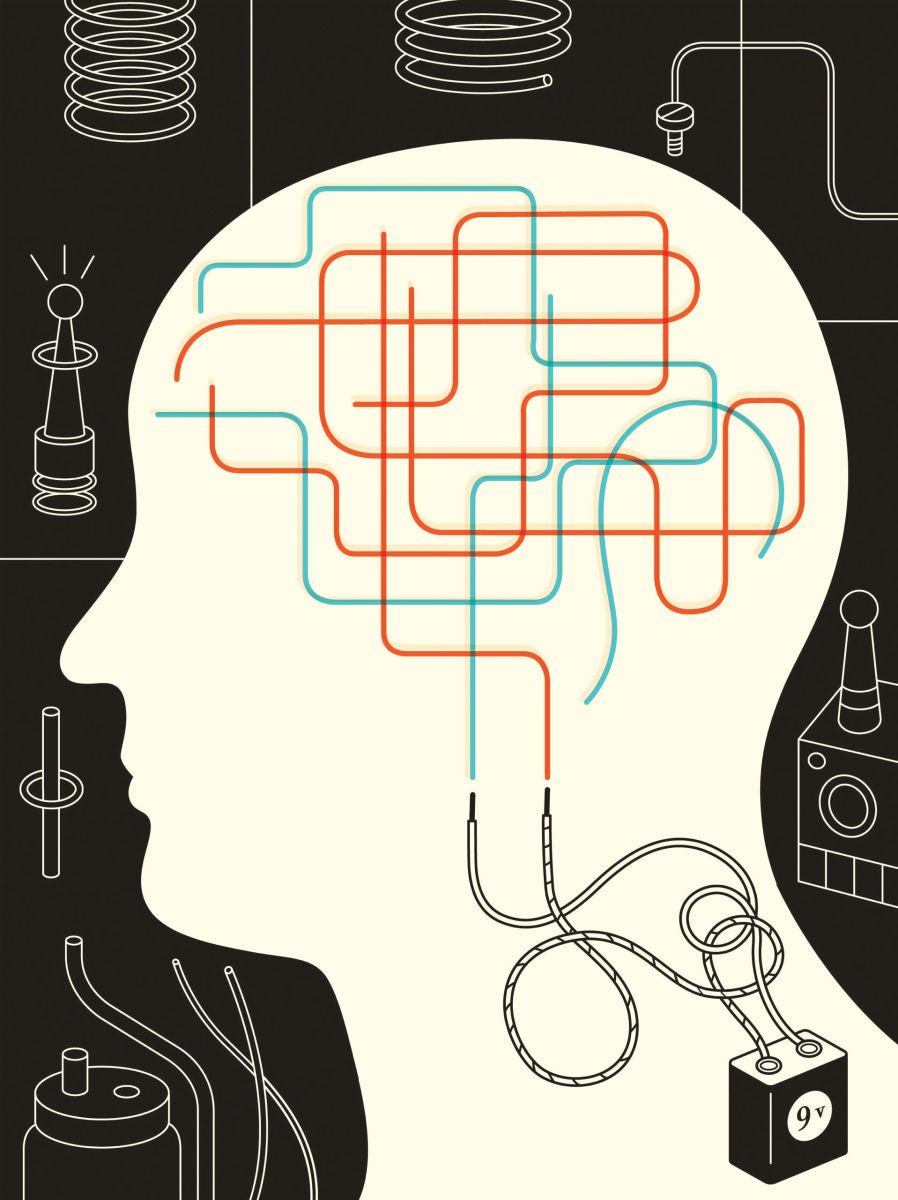
Photo Credit: Harry Campbell/New Yorker Several studies have found transcranial direct-current stimulation (tDCS) to lead to improvements in working memory, learning, decrease depression, alleviate chronic pain, and reduce symptoms of Parkinonson’s and schizophrenia. A recent article in the New Yorker describes a journalists journey undergoing tDCS and her discussions with those in the field:
“What does this part of the brain do, again?” I asked, pointing to the electrode on my right temple. “That’s the right inferior frontal cortex,” said Vince Clark, the director of the University of New Mexico Psychology Clinical Neuroscience Center, in Albuquerque. “It does a lot of things. It evaluates rules. People get thrown in jail when it’s impaired. It might help solve math problems. You can’t really isolate what it does. It has emotional components.”
It was early December, and night was falling, though it was barely five. The shadows were getting longer in the lab. My legs felt unusually calm. Something somewhere was buzzing. Outside the window, a tree stood black against the deepening sky.
“Verbal people tend to get really quiet,” Clark said softly. “That’s one effect we noticed. And it can do funny things with your perception of time.”
The device administering the current started to beep, and I saw that twenty minutes had passed. As the current returned to zero, I felt a slight burning under the electrodes—both the one on my right temple and another, on my left arm. Clark pressed some buttons, trying to get the beeping to stop. Finally, he popped out the battery, the nine-volt rectangular kind.
This was my first experience of transcranial direct-current stimulation, or tDCS—a portable, cheap, low-tech procedure that involves sending a low electric current (up to two milliamps) to the brain. Research into tDCS is in its early stages. A number of studies suggest that it may improve learning, vigilance, intelligence, and working memory, as well as relieve chronic pain and the symptoms of depression, fibromyalgia, Parkinson’s, and schizophrenia. However, the studies have been so small and heterogeneous that meta-analyses have failed to prove any conclusive effects, and long-term risks have not been established. The treatment has yet to receive F.D.A. approval, although a few hospitals, including Beth Israel, in New York, and Beth Israel Deaconess, in Boston, have used it to treat chronic pain and depression.
“What’s the plan now?” Clark asked, unhooking the electrodes. I could see he was ready to answer more questions. But, as warned, I felt almost completely unable to speak. It wasn’t like grasping for words; it was like no longer knowing what words were good for.
Clark offered to drive me back to my hotel. Everything was mesmerizing: a dumpster in the rear-view camera, the wide roads, the Route 66 signs, the Land of Enchantment license plates.
After some effort, I managed to ask about a paper I’d read regarding the use of tDCS to treat tinnitus. My father has tinnitus; the ringing in his ears is so loud it wakes him up at night. I had heard that some people with tinnitus were helped by earplugs, but my father wasn’t, so where in the head was tinnitus, and were there different kinds?
“There are different kinds,” Clark said. “Sometimes, there’s a real noise. It’s rare, but it happens with dogs.” He told me a story about a dog with this rare affliction. When a microphone was placed in its ear, everyone could hear a ringing tone—the result, it turned out, of an oversensitive tympanic membrane. “The poor dog,” he said.
We drove the rest of the way in silence.
Growing up in Detroit, Clark was interested in philosophy and thought he would study it in college. But, after realizing that all the questions that interested him came down to perception and the brain, he majored in psychobiology, at U.C.L.A. This was in the nineteen-eighties. “By luck, I picked a field that was about to explode,” he said.
As an undergraduate, Clark took a job at a hospital, building electrodes for insertion into the brains of epileptics during surgery, to locate the epileptic regions of the brain and the regions necessary for cognitive function. The patient’s head would be sawed open under local anesthetic. Fully conscious, the patient would be shown flashcards with words or pictures while the electrodes recorded which regions responded to the stimuli. Clark was deeply impressed by how localized neuronal responses were. Sometimes, a picture of a particular celebrity would cause a single neuron to become especially active. Similar observations led scientists in a later study to posit the existence in one patient of a “Halle Berry neuron.”
Just before Clark got his Ph.D., the fMRI machine was developed—a huge moment for neuroscience. The technology measures brain activity in real time, by monitoring blood flow. Scientists today can look at an fMRI and see what happens in the brain of a pianist playing Bartók, a Carmelite nun having a religious experience, a depressed person contemplating suicide, or a schizophrenic hearing voices. As a professor at the University of Connecticut Health Center, Clark began working on an addiction study, using fMRI to look at the brains of recovering addicts. To his surprise, he noticed that the fMRI could show which of the recovered addicts were likely to relapse in six months. Clark believes that it may be possible to stimulate a relapser’s brain with tDCS to make it look and act more like a non-relapser’s.
The precise physical mechanism of tDCS remains mysterious. The electric current used is too low to cause resting neurons to fire. Instead, it seems to make neurons more or less likely to fire, by changing the electrical potential of nerve-cell membranes. In other words, although tDCS can’t create new neural activity, it can enhance or reduce existing activity. The procedure uses direct current, so it has positive and negative electrodes and can have both inhibitory and excitatory effects: in general, positive current stimulates neural activity while negative current inhibits it.
Clark began working on tDCS in 2007, shortly after being named scientific director of the Mind Research Network at the University of New Mexico. Funded by DARPA, the research division of the Department of Defense, his first study determined that tDCS can help subjects learn to detect hidden threats in complex images. The researchers used images from DARWARS, a video game designed to familiarize Army recruits with the desert roads, derelict apartment blocks, and abandoned fruit markets that are apparently typical of the Middle Eastern landscape. For most people, the concealed threats—an explosive device hidden behind an oil drum; the shadow of a sniper’s rifle protruding over a rooftop—can be identified only with training and practice. At the beginning of the study, subjects’ brains were scanned by fMRI while they received training, to show which regions were active during learning. These areas were then targeted by electrodes in a new group of subjects as they performed the same task. Half of them received active tDCS; the other half, the control group, received “sham tDCS”—a negligibly low dose.
To Clark’s disbelief, the subjects who received tDCS learned the same material twice as quickly as the control group. The study was replicated by other labs, with similar results. The Air Force found that tDCS made airmen twice as accurate at identifying tanks and missile launchers in radar scans.
“It’s a huge, huge effect,” Eric Claus, a neuroscientist at the Mind Research Network, told me of the original results. “As cognitive neuroscientists, we rarely see effects that large.”
On hearing of Clark’s findings, Claus decided to incorporate tDCS into his own work: the treatment of alcoholism using cognitive exercises. He is currently replicating a study in which alcoholics were found to drink less after repeatedly using a joystick to push away images of beverages. Claus scans the brains of alcoholics while they perform the joystick task; he then uses tDCS to stimulate the active regions on a new group of alcoholics. Two members of the tDCS group have gone from drinking a fifth of liquor a day to not drinking at all.
Few claims about tDCS are free from controversy. In the past few months, Jared Horvath, a fourth-year doctoral student at the University of Melbourne, published two meta-analyses of hundreds of studies, in which he claims to have found no evidence of either physiological changes to the brain or of cognitive effects from tDCS. In aggregate, Horvath says, the claims of different researchers tend to “cancel each other out.” For instance, four studies looked at whether tDCS increased glucose metabolism in the brain: two found that it did; two found that it didn’t. “It’s incredibly difficult to differentiate these effects from random chance,” Horvath told me.
Horvath spent his first two years of graduate school trying unsuccessfully to get meaningful results from tDCS. “It didn’t matter what device I used, what paradigm I used—I just never found anything,” he said. The original purpose of his meta-analyses was simply to identify a reliable tDCS effect to use as a dissertation topic. Though skeptical, Horvath isn’t saying that research should be abandoned. Rather, he argues that the focus must shift from documenting various individual effects to establishing the reliability of a baseline effect through large randomized studies with standardized protocols—a view shared by most researchers.
On my second day in Albuquerque, I met with three of Clark’s researchers to try tDCS again, with a cognitive task. This time, the current would stimulate “location F4,” an area of the scalp that lies over a part of the brain associated with working memory. Two students measured my head with a tape measure and fed the information into a software program, which told them how to find F4 relative to my ears. As they were annotating my head with colored stickers, I noticed a white ceramic phrenological bust standing on the desk. Its face wore a vacant yet weary expression, and its cranium was mapped with what phrenologists had considered to be the most basic human propensities: Wonder, Parental Love, Calculation, Secretiveness. I tried to gauge the place corresponding to F4, on the top right part of the head. It seemed to be near Sublimity, or Hope.
There was some trouble getting the gel-saturated sponge electrode to stay put on my hair. The students wrapped a band of elastic netting around my head, and I held it in place with one hand. Throughout the study, I could feel the band oozily creeping up the back of my skull, like an ill-fitting graduation cap.
With the current off, I took two memory-related tests. In the first, the n-back test, a series of letters flashed on a screen, and I was told to decide whether each letter was the same one that flashed three letters ago. Next was a “progressive matrices” test, which involved choosing a visual pattern that matched a matrix of other patterns. After I had completed the tests, both of which I found difficult and annoying, the students turned on the tDCS. I felt a burning on F4 as the current ramped up. (A burning or tingling sensation or a metallic taste in the mouth is a common side effect, though some people don’t feel anything at all.) I took the n-back test a second time. It was slightly less annoying and seemed to go by a bit faster. Then they turned the current off, and I took the matrices test again. It seemed a little bit easier than the first time, and I felt more peaceful, but, perhaps as a result of the peaceful feeling, I ran out of time and was unable to answer two questions.
Afterward, I learned the point of the study. Previously the experimenters had found that tDCS improved performance on the n-back test. Now they were trying to determine whether the benefit was “transferrable” to a different memory-related test once the current was switched off. In my case, the answer was no: I got exactly the same score—three out of nine—both times. The students didn’t seem that surprised. They hadn’t been getting great results. “You shouldn’t feel bad,” one of them said, handing me a tissue to wipe the gel off my hair. “Some people don’t get any of them right.”
The next morning, I returned to the psychology department to try tDCS a third time. I met with Katie Witkiewitz, a U.N.M. psychologist, who recently began incorporating tDCS into her work on addiction, meditation, and mindfulness. In earlier studies, Witkiewitz and her colleagues found Vipassana, a Buddhist meditation practice, to be more effective at preventing drug relapse than either cognitive behavioral therapy or twelve-step programs. She is now embarking on research to determine if tDCS can make a meditative state deeper, easier to achieve, and longer-lasting—an attractive prospect for those who, like me, find meditation too boring and frustrating to practice with any regularity.
Witkiewitz put an anode over my right temple. In a trancelike tone, she instructed me to think about my breath, to imagine a balloon slowly filling in the empty space behind my eyes, to focus all my attention on the area directly above my head. She told me to watch my thoughts come and go. In previous attempts at meditation, I had always found this the hardest instruction to follow. My feeling was that either I was thinking my thoughts or I wasn’t. If I was thinking them, I wasn’t watching them. If I was watching them, I wasn’t thinking them.
This time, I noticed that I thought, If there were really a balloon in my head, you, neuroscientist, would be out of a job. And then, as instructed, I let the thought drift away. Although there is no quantitative test to measure the depth of a meditative state, I felt that my thoughts were, for a few hours afterward, calmer, more manageable, more countable—like a few sheep standing in a pasture instead of some demented sheep convention. My mind felt quieter, as if an inner voice had gone silent—the voice that usually says, “This is stupid, it’s a waste of time, why isn’t it over?”
Some tDCS studies have involved “quieting” a part of the brain by inhibiting neural activity. An Australian group, writing in Scientific American, claims that using tDCS to inhibit left-hemisphere brain activity improves performance on certain logic problems. The authors were inspired by the “savant skills” that sometimes accompany brain damage—as in the case of a boy who, having been shot in the head, lost the ability to read and write but became able “to dismantle and reassemble multi-gear bicycles without instruction,” raising the possibility that extraordinary skills may be “latent in us all.”
The authors’ study of special skills displayed by patients with autism and brain damage hints at one area of concern regarding tDCS: with brain function, as with most things, you rarely get something for nothing. As Roi Cohen Kadosh, a neuroscientist at Oxford University, puts it, “Enhancing one cognitive ability can happen at the expense of another ability.” Cohen Kadosh, the editor of a textbook called “The Stimulated Brain,” has found that applying tDCS to one part of the brain helped subjects learn a math-related task but impeded their ability to recall what they had learned.
Heidi Schambra, a Columbia University neurologist who uses tDCS in her research with stroke patients, cautions against the view of tDCS as “a ‘thinking cap’ where you just put it on and everything becomes easier.” Some stroke patients recover motor function more quickly when tDCS is administered during physical therapy—but without physical therapy tDCS doesn’t seem to have any effect, and even with the therapy the effects aren’t huge. “We’re not seeing a tripling or quadrupling,” Schambra said. “It’s a few points of statistical difference.”
The human drive to zap one’s head with electricity goes back at least to antiquity, and was originally satisfied by means of electric fish. “Headache even if it is chronic and unbearable is taken away and remedied forever by a live torpedo placed under the spot that is in pain,” the first-century physician Scribonius Largus wrote. He also used the torpedo, a species of ray native to the Mediterranean, to treat hemorrhoids. In the eleventh century, the Islamic polymath Avicenna reportedly recommended the placement of an electric catfish on the brow to counteract epilepsy. As late as 1762, a Dutch colonist in Guyana wrote that “when a slave complains of a bad headache” he should put one hand on his head and another on a South American electric eel and “will be helped immediately, without exception.”
The invention, in 1745, of the Leyden jar—a device to store static electricity—enabled many new experiments in electrotherapy, not all of them deliberate. In 1783, Jan Ingenhousz, a Dutch scientist, accidentally picked up a charged Leyden jar, causing an explosion that made him temporarily lose his memory, judgment, and ability to read and write. Having found his way home with great difficulty, he went to sleep. He woke to find that his mental faculties had not only returned but had sharpened: “I saw much clearer the difficulties of every thing,” he wrote in a letter to Benjamin Franklin. “What did formerly seem to me difficult to comprehend, was now become of an easy solution.”
Around the same time, Luigi Galvani’s experiments with electricity and dead frogs led to the discovery of bioelectrical impulses. Galvani’s nephew Giovanni Aldini was the first to apply galvanic current to humans; in this way he seemingly reanimated the corpses of beheaded felons. One such demonstration, at London’s Royal College of Surgeons, may have inspired Mary Shelley’s invention of Frankenstein’s monster.
Electrotherapy on living people gained popularity in the nineteenth century. By 1850, European and American asylums used galvanization to treat hysteria, menstrual pain, depression, and psychosis. Machines for electrotherapy were sold in London department stores and leased at seaside resorts. An 1871 electrotherapy textbook outlines treatments for hundreds of conditions, such as alcoholism, paralysis, dyspepsia, mutism, and “neurasthenia”—a form of nervous exhaustion that later came to be known as Americanitis. Many of the case histories in the book involve a procedure that sounds much like tDCS: direct current is applied by sponge electrodes, with a common side effect of “intense redness and an acute burning sensation.” After such “galvanization,” patients often “find that they can read with closer attention and with greater zest; that they can pursue connected thought without fatigue, and endure mental toil and anxiety that was once intolerable.”
In the twentieth century, electrotherapy gradually fell from favor. Freud, who studied it with the neurologist Jean-Martin Charcot in Paris, abandoned it in favor of the “talking cure,” after returning to Vienna. During the First World War, electricity was used to treat paralysis, epilepsy, and shell shock, often with disastrous results. In Louis-Ferdinand Céline’s “Journey to the End of the Night” (1932), the hero receives a diagnosis of low patriotism and is sent to a military psychiatric hospital, where, he recalls, “they pumped us full of shocks.” Electroconvulsive therapy (ECT), which uses a far higher current than tDCS to trigger a full-brain seizure, gained in popularity by the nineteen-forties, but was generally considered a last resort for only the most serious cases. After the Second World War, interest shifted to antidepressants and other psychotropic drugs.
The decline of electrotherapy coincided with the rise of brain imaging. The first milestone was the invention, in 1924, of the electroencephalograph (EEG) by Hans Berger, an enigmatic figure who may later have coöperated with the Nazi government, and who hanged himself in 1941. The EEG, which measures electrical discharge from the brain, was the first in a series of technologies to show that the brain physically changes depending on what we do, think, and feel, and that the brains of the mentally ill function differently from those of the healthy.
Berger’s innovation had its roots in his interest in psychic phenomena. As a young man in the Prussian Army, Berger once fell off a horse and was almost run over by an artillery gun. The previous night, his sister, to whom he was very close, had dreamed that he fell off a horse and broke his leg. The sister was so alarmed by the dream that she had their father send Berger a telegram; it reached Berger immediately after his accident. Berger was convinced that his brain had sent electrical signals to his sister. And he was right, almost: the brain does generate electrical impulses, and they change depending on your mental state. Though too weak to travel through the air, they may be recorded by electrodes placed on the scalp. Your brain can’t tell your faraway sister that you’re about to fall off a horse, but it can tell an EEG machine that you’re frightened or having a seizure or asleep.
The resurgence of interest in electrical brain stimulation began in 2000, after scientists in Göttingen proved that low-current “galvanization,” the procedure now known as tDCS, could change brain function. This discovery coincided with a wave of interest in neuroplasticity—the brain’s capacity for change—and with the rise of increasingly sophisticated imaging tools, like fMRI. The number of tDCS studies has risen steadily since 2000, with more than four hundred studies published last year.
Perhaps the most dramatic clinical use of tDCS has been in the treatment of auditory hallucinations. In Albuquerque, Clark introduced me to Jaime Campbell, a forty-year-old woman who has been hearing voices since she was fifteen, and who recently participated in a study at U.N.M. Heavyset, with a placid and cheerful demeanor, she was carrying a crochet project in a tote bag labelled “Bible Bag.” The first voice she had ever heard, she said, was the voice of God. She had been sitting at a computer table at the time, and God said she would go to South Africa and die a martyr. At sixteen, Campbell began to be followed by the man she called “the chaperon.” He walked six feet behind her, and would rape and kill her if she did anything wrong. “I didn’t cuss. I didn’t lie. I didn’t cheat. I didn’t even say the word ‘sex,’ ” Campbell recalled. “I was a very well-behaved teen.”
At nineteen, Campbell was given a diagnosis of schizophrenia. People asked her then why she had never mentioned the chaperon. “Because it was normal,” she said. “Every sixteen-year-old has a chaperon.”
An estimated seventy-five per cent of schizophrenics hear voices, and twenty-five to thirty per cent of those cases don’t respond to medication. The majority of the voices are nasty, telling subjects that they are worthless or should commit suicide. Campbell told me that her voices all belong to men, with the exception of one “non-gendered voice” that used to talk about her in the third person. “She’s stupid,” it would say. “No, she’s not stupid—she’s ugly. She’s not ugly—she hatespeople. She doesn’t hate people—they hate her.” Once, the voices said that anyone she spoke to would explode. She didn’t speak a word for three days and nights, to keep everyone safe.
Campbell’s other symptoms have included visual hallucinations and delusions of persecution. Once, she saw four demons—red misshapen creatures with tails—hanging up near the ceiling in the four corners of the room, watching her. Campbell was raised in a nondenominational charismatic church, and religion is still extremely important to her. She believes that she’s more in touch with the spiritual world than most people and that the visions and voices come to her from God. But she also believes that her mind “twists things,” that it causes her suffering beyond what’s ordinary or bearable.
For the past twenty years, Campbell has been in treatment with medications and with ECT, which helped with her depression but didn’t silence the voices. Last summer, she began an experimental treatment offered by Clark and Robert Thoma, a U.N.M. psychologist who specializes in schizophrenia. The trial is based on a randomized study done in France in 2012, in which thirty schizophrenics were given tDCS for five days. The treatment decreased auditory hallucinations by thirty-one per cent, and the benefits lasted, and in some cases grew, over the next three months.
Campbell received two twenty-minute tDCS sessions a day for five days. After the very first session, she felt a reduction in the “tea party”: an ambient murmuring and clinking that she always heard in the background. Gradually, particular voices went mute. By midweek, Campbell says, her head was completely quiet.
“I never had a response like tDCS,” Campbell says. “Even with the ECT, even with the best medication combinations that we’ve come up with, I’ve never had something that does as complete a job.” Unlike ECT, which lost effectiveness over repeated treatments, tDCS seemed to help more and more, even after the study had ended. For weeks, Campbell didn’t hear any voices at all. Everything became easier: thinking, grocery shopping, driving a car. The most revolutionary thing, she says, was “to not have someone constantly telling me that I’m a horrible person.” People used to tell her that she was a good person, but she never believed them, because the voices said the opposite—and didn’t they know her best? When they finally shut up, she said that she felt like a woman who had been rescued from an abusive husband.
Clark and Thoma will eventually replicate the randomized controls of the French experiment, but so far Campbell is one of only two people to have completed their study, and the fluctuating nature of schizophrenia symptoms makes it dangerous to infer too much from her experience. When I met her, four months had passed since her last tDCS session. The voices had started to return, though only sporadically. Over the weekend, she had heard a voice at Walmart telling her she was a bad person and that people were going to blow her up. But when she left Walmart the voice went quiet. She still feels better than she did before the study. But every time she hears a voice she feels terrified that “they’re going to come back full-fledged.”
Before tDCS can be approved by the F.D.A. and enter widespread use, there have to be large randomized controlled trials. Protocols must be standardized—the placement of the electrodes, the amount of current, and the duration, frequency, and number of sessions. In the meantime, there is a device called ActivaDose, which has been cleared by the F.D.A. for another purpose (administering drugs transdermally), and which can also administer tDCS; physicians may legally prescribe it “off label,” which is how some hospitals can offer the therapy. Several Internet companies sell tDCS kits for nonmedical uses, such as boosting cognition or enhancing video-game performance. There is a tDCS subreddit, a do-it-yourself tDCS blog and podcast, and a certain amount of YouTube footage showing young men with little scientific background zapping their brains in the hope of learning German or playing better chess.
It is the rare human who doesn’t wish to change something about his or her brain. In my case, it’s depression, which runs on both sides of my family. I’ve been taking antidepressants for almost twenty years, and they help a lot. But every couple of years the effects wear off, and I have to either up the dose or switch to a different drug—neither process can be repeated indefinitely without the risk of liver or kidney damage. So although my symptoms are under control for now, I worry, depressively, about what will happen when I exhaust the meds. As I was researching this piece, my attention was caught by a number of randomized controlled trials showing a benefit from tDCS for depression. (The data are insufficient to allow definitive conclusions, but larger trials are in progress.) I was almost embarrassed by how excited I felt. What if it was possible to feel less sad—to escape the deterministic cycle of sadness? What if you could do the treatment yourself, at home, without the humiliation and expense of doctors’ visits? I asked Vince Clark whether any private physicians use tDCS outside of a research setting.
He knew of only one: James Fugedy, a Yale-trained anesthesiologist who practices in Atlanta. I spoke with Fugedy on the phone and learned that, since 2007, he has treated between three hundred and four hundred patients with tDCS, principally for chronic pain and depression. Most of his patients self-administer tDCS at home: Fugedy charges twenty-six hundred dollars for a package including the device, a diagnostic and training session, and follow-up consultations in person or over Skype.
Early this year, I took a plane to Atlanta. Fugedy’s practice is in a medical park about half an hour from the airport. The sign on the suite door—“Brain Stimulation Clinic”—seemed to suggest a large staff, but the only people there were Fugedy and a dreadlocked office manager in scrubs.
Fugedy, a sixty-five-year-old New Jersey transplant, combines a soft-spoken demeanor with boundless energy. He told me that he first learned about tDCS from a 2006 study on fibromyalgia, published by scientists at Harvard. He mentioned the paper to a patient, saying he hoped that the F.D.A. would approve the technology soon. “I’m old,” she replied. “Why can’t we do it now?”
Fugedy practiced tDCS a few times on himself and then began to treat his fibromyalgia patient. After five sessions, she experienced a greater reduction in pain than she had on any other treatment. Fugedy went on to use the tDCS with other chronic-pain patients. In 2008, he got a call from a chronically depressed electrical engineer in southern Georgia. His doctor had prescribed ECT, but he was worried about possible memory loss; he had heard of tDCS, and wanted to try it first. Fugedy agreed, and the engineer began commuting to Atlanta five days a week. After four weeks, his mood had improved, and he stopped the treatment. Three months later, when the symptoms returned, Fugedy got him his own stimulator and showed him how to use it.
Fugedy’s recent patients include a bipolar pregnant woman who couldn’t take her medications during pregnancy and a thirty-year-old schizophrenic man who had been unable to tolerate antipsychotics. After starting tDCS, Fugedy told me, the man was able to get his first job and enroll in college. Fugedy, who has had depressive episodes himself, has been self-administering tDCS on and off for eight years.
After we had been talking for an hour or two, Fugedy handed me a black plastic case about the size of a desk dictionary. Inside were two electrodes with cables and sponges, a nine-volt battery, a Velcro headband, and an ActivaDose. He showed me how to wet the sponges, fit them into the frames, and connect the electrodes to the stimulator.
Fugedy thinks that the electrodes move around less if you lie down, so I lay on the examination table and slipped the electrodes underneath the Velcro headband. The anode went just over my left eye, to stimulate the left dorsolateral prefrontal cortex—a part of the brain that may be underactive in depressed people—and the cathode over the visual cortex, on the back of my head. Then I set the timer for twenty minutes and the current to two milliamps, and turned the dial to start the flow of electricity. As the current ramped up, I felt the familiar burning on my forehead and general wordlessness.
For a short time, Fugedy kept up his end of a conversation we had been having about neuroimaging. “Well, I’ll just leave you in peace,” he concluded eventually, handing me a brass handbell and leaving the room.
Sun shone in a halo around the corner of the window blinds. On the wall hung a picture of a woman cradling a naked infant; a pair of white wings sprouted from the child’s tiny shoulders. A cursive caption read “Hope Cherishing Love.” I felt obscurely troubled by the caption. Wasn’t it love that cherished hope, rather than the other way round? Wasn’t hope the thing with feathers? The longer I thought about it, the more the words resisted understanding and shifted places, again and again, like markers on a game board. My thoughts turned to the many patients who must have lain on this same white table and held this same brass bell, and how appropriate the image of hope was, because surely nobody would be here if he hadn’t tried a lot of other things first.
I felt peaceful in the cab back to the airport. The T.S.A. didn’t try to confiscate the nine-volt battery. On the plane, I was seated beside a small girl who was playing a game called Office Jerk on her iPad. The game involved throwing a stapler at the head of an office worker. “Who’s the jerk, him or you?” the girl’s mother asked. I wondered if I should offer to improve the girl’s performance with a little stimulation to the right inferior frontal cortex, but she didn’t appear to need it.
The next day, I tried tDCS at home. I felt some burning again and tightened the strap; Fugedy had said this might improve the electrode connection. It’s possible that I overdid it with the tightening, because at the end of twenty minutes I had a pink electrode-shaped square on my forehead. In the shower afterward, I felt my forehead sting under the hot water, as if sunburned. A headache that had come on at some point during Office Jerk was now insistently throbbing behind my left eyebrow. Yet, whether because of the tDCS or for some other reason, I was in excellent spirits the rest of the day, and indeed all week. (The pink square went away within minutes; the headache lingered for days.) The fact that I might have suffered a mild burn on my forehead because of a brain-zapping machine I had bought in Atlanta seemed hilarious. It was a new year, fresh snow had fallen, the holidays were finally over. New York looked beautiful.
My plan to try tDCS for two weeks, to see if it made a difference in my depression, fell through for an unexpected reason: I didn’t feel depressed enough. It was a reminder, if I needed one, of how difficult it is to extract scientific facts from human experience. Even when you isolate one variable and test it in a lab with control subjects, it’s difficult to know why you’re seeing what you see; and in the messiness of everyday life, where there are any number of reasons that your mood might change from one week to the next, it’s virtually impossible to gauge the effects of applying subthreshold electricity to your own head.
One of the mysteries of tDCS is why some uses require a cognitive task and others don’t. The therapy makes people better at math only if it’s paired with a math task. But it seems to make depressed people feel better even if they’re just sitting there. Heidi Schambra, the neurologist who works with stroke patients, has a fascinating theory about this. She believes that, at the moment of receiving tDCS, a person in emotional or physical pain is engaged, wittingly or unwittingly, in a cognitive task: namely, the activation of the placebo response.
We’re not used to viewing placebo—a positive response to a sham treatment—as a “task,” but there are many cognitive factors involved, including Pavlovian conditioning, the patient-clinician relationship, and positive expectation. Deception, Schambra points out, may not be required: sugar pills have been shown to reduce the symptoms of irritable bowel syndrome, even in patients who were explicitly told that they were receiving a placebo.
The implication of placebo is extremely powerful: What if the body knows, in some sense, how to heal itself, and it’s just a matter of triggering that knowledge? Schambra suspects tDCS may not merely trigger the placebo effect, as all treatments do, but actually amplify it. In other words, in a controlled tDCS study, both active and sham groups get a placebo effect, but the active group may get a bigger effect. Schambra emphasizes that her theory is just speculation for now. She got the idea from a study that found expectancy to be an important factor in how well people responded to depression treatment: the patients who felt better were the ones who expected to feel better—not necessarily the ones who got the active versus the placebo treatment.
After we hung up, I found myself thinking about what neurologists call “positive expectancy” and what the phrenologists called hope. The phrenologists already knew that hope was situated in the prefrontal cortex: “in front of conscientiousness, and behind marvelousness, being elongated in the direction of the ears.” Phrenologists were unable to detect hope in animals; in criminals, they said, it was diminished. Hope inspires and dupes us in turn, eternally promising happiness in this world and the next. In a lecture on phrenology, the French physician Broussais once produced a partial mold of Napoleon’s head. You couldn’t see everything, he said. But you could see enough of the organ of hope to conclude that it was very well developed.
Read the original article Here
- Comments (0)
- Brain Networks in People with Autism
- By Jason von Stietz
- April 3, 2015
-

Photo Credit: Getty Images The human brain is composed of trillions of neurons, which interact to form complex signaling networks. Researchers at the University of Miami have examined how these networks are differ in the brains of people with autism as compared to the brains of typically developing people. A recent article in NeuroScientistNews discusses the study:
The field of autism research has tried to find a central theory underlying brain changes associated with autism spectrum disorder (ASD). Now, a new study shows that individuals with the disorder exhibit different patterns of brain connectivity, when compared to typically developing (TD) individuals and that these patterns adjust as the individual ages.
"Our findings suggest that developmental stage must be taken into account to accurately build models that show how the brains of individuals with autism differ from neurotypical individuals," said Lucina Uddin, assistant professor of Psychology at the University of Miami (UM) College of Arts & Sciences and corresponding author of the study. "We believe that taking a developmental approach to examining brain connectivity in autism is critical for predicting response to treatment in young children with ASD."
Our brain is composed of more than one trillion neurons, interacting with one another to form complex signaling networks. Previous studies have identified patterns of both functional hypo- and hyper-connectivity of these signaling networks in individuals with ASD. The current study, titled "Developmental Changes in Large-Scale Network Connectivity in Autism," attempts to explain these conflicting results, by indicating that the developmental stage of the individual plays a key role in the findings. The study is published in the journal NeuroImage: Clinical.
Key findings of the study include:
♦ Children (7 to 11) with ASD, exhibit hyper-connectivity within large-scale brain networks, as well as decreased between-network connectivity, when compared to TD children.
♦ Adolescents (age 11 to 18) with ASD do not differ in within network connectivity, but have a decrease in between network connectivity, from TD adolescents.
♦ Adults (older than 18) with ASD show neither within, or between-network differences in functional connectivity compared with typical adults.The findings suggest that alterations in the networks of the brain's cortex may trigger the complex behavioral characteristics observed in individuals with ASD.
"This study helps us understand the functional organization of brain networks and how they change across the lifespan in autism," said Jason S. Nomi, postdoctoral fellow in the Department of Psychology at UM and lead author of the study.
The researchers are currently working to explicitly characterize an important developmental transition in individuals with autism: the onset of puberty.
Read the original article Here
- Comments (0)


 Subscribe to our Feed via RSS
Subscribe to our Feed via RSS