Blog
- Transcranial Magnetic Stimulation: A Non-Drug Treatment Option for Depression
- By Jason von Stietz
- July 29, 2015
-

Photo Credit: Getty Images It is estimated that 7 percent of people in the United States live with clinical depression. Transcranial magnetic stimulation (TMS), involves stimulating the prefrontal cortex, which is found to be under-activated in people with depression. TMS is a non-drug treatment option that is beginning to find favor among clinicians and researchers, alike. A recent article in the Tribune discussed the empirical research and the experience of clinicians supporting TMS:
Depression lifted from Nick O'Madden's life like a set of foggy glasses being wiped clean.
Earlier this summer, O'Madden, 31, felt he was living in a distracted haze, sprinkled with nighttime panic attacks. Now, after undergoing an emerging high-tech treatment involving magnetic currents, he said he's literally seeing the world in a new light.
"Colors are brighter," said O'Madden, a mental health therapist who lives in Elk Grove, Calif. "Last night, I was looking at the moon, and it just looked clearer and brighter and more beautiful ... It's almost kind of scary to see that at first, it's so new to me."
He described the changes from a reclined medical chair at TMS Health Solutions, a treatment center in Sacramento's Campus Commons area that specializes in transcranial magnetic stimulation. With a metal coil positioned near his forehead, he spoke between bouts of jackhammer-esque pulsing that erupted every 15 seconds during the 50-minute session.
The "train pulses," as technicians call the strings of sound, are actually the back-and-forth flexing of the metal coil as the device sends out a 2-tesla-strong magnetic current. The coil creates a magnetic field that reaches 2 to 3 centimeters into brain matter to stimulate the dorsal-lateral prefrontal cortex, the poker chip-sized area responsible for regulating mood, memory and decision-making.
An estimated 7 percent of American adults suffer from clinical depression, which can cause lethargy, indifference, moodiness and other symptoms that interfere with day-to-day functioning. Researchers have found that the prefrontal cortex is often underactive in people diagnosed with the illness.
The TMS technology uses electric currents to excite cell activity in that part of the brain, theoretically helping neurons better communicate with one another and increasing blood flow to the tissue, which promotes healthy brain function. The federal Food and Drug Administration has approved the treatment, but for limited use given that it is relatively new. Physicians can administer it only to patients who haven't responded to at least one prescription medication for depression.
Advocates of the treatment refer to it as revolutionary; there hasn't been a major development in procedure-based depression treatment since the advent of electroconvulsive therapy. Unlike that treatment, which applies electricity directly to the skull to invoke a brain seizure, the magnetic TMS procedure has not shown negative impact on memory or cognition.
TMS, and other new treatments that focus on physical stimulation of specific parts of the brain, signal a departure from traditional methods of treating mental illness, such as talk therapy and prescription drugs. As advances in medical technology allow researchers to better understand how the human brain functions, approaches to treatment are following suit.
"There's a growing recognition, both with scientists and patients, that depression is a brain problem - a problem with chemicals in our circuitry," said Dr. Paul Croarkin, a psychiatrist with the Mayo Clinic. "The fact that we're soon going to have more and more offerings in that regard is a positive thing."
As with many emerging medical treatments, practitioners and insurers hesitate to embrace new procedures without a solid track record. Though the FDA approved the nation's first TMS device in 2008, major health insurance companies have only begun covering the treatment in the past few years.
Dr. Richard Bermudes is principal owner and medical director of TMS Health Solutions and president of the nationwide Clinical TMS Society. By his estimate, about 700 TMS devices are in use in the United States.
The treatment has been the focus of about 30 randomized clinical trials in the United States, and in most of those, a statistically significant portion of patients were determined to have benefited. But some researchers caution that the improvements could be the result of a placebo effect, and have called for longer-term studies.
A 2012 study published in the Journal of Clinical Psychiatry showed that half of the patients involved in that trial responded to the treatment within six weeks, and 25 percent went into remission. Still, guidelines from the Agency for Healthcare Research and Quality and the Department of Health and Human Services state that evidence is "insufficient to evaluate the ability of (repetitive) TMS to maintain response or remission."
On the upside, the therapy has not been shown to cause whole-body side effects, such as weight gain or fatigue, as an oral medication might, said Dr. Guohua Xia, a clinical associate professor at University of California-Davis and medical director of Brainefit, a mental health institute offering a form of TMS services. That means it can be especially helpful for pregnant women and elderly people who may experience problems with standard depression drugs.
Sutter Health is the only hospital system in Sacramento to offer the treatment. Dr. Theodore Goodman, director of interventional psychiatry for Sutter Health, said TMS has resulted in improvement for about 60 percent of patients during the two years it has been offered at the Sutter Center for Psychiatry.
He expressed frustration at insurance companies not covering the treatment long term. TMS is currently approved only as a treatment for acute clinical depression, meaning patients are in the throes of symptoms.
"About 50 percent of patients will relapse over a year's time," he said. "The way you avoid that is maintenance treatment, but insurance won't pay for that. It's a horribly unenlightened viewpoint."
While NeuroStar, the model used at Bermudes' clinic, was the first TMS device approved on the market, other brands go even further into brain matter and have been used to target other conditions, including migraines.
At TMS Health Solutions, the recommended treatment plan is four to six weeks of daily TMS sessions, at a cost of $5,000 to $7,000. Since opening clinics in El Dorado Hills, Calif., in 2007 and Sacramento in 2010, Bermudes said, he has used the technology to treat hundreds of patients and currently sees about 20 TMS patients a day.
He said he recently changed the clinic's name - from Mindful Health Solutions - specifically to highlight the treatment.
"There's not a lot of access to this modality currently in the community," he said. "A lot of our patients have been depressed for years before coming to TMS. If we can get people into TMS earlier, our remission and response rates may go up."
O'Madden said that, for him, improvement came after three weeks of treatment, though technicians say results can take longer. Before his physician suggested TMS, O'Madden said, he was having trouble sleeping and focusing, and struggled to control anxiety and obsessive thought patterns.
He said he's now feeling more focused and active, with a renewed passion for boxing. He recently started a blog to document his recovery.
"I want people to become more aware of (TMS), and I also want mental health to be less stigmatized," he said. "I want people to see me as a person: I'm a father and a husband, but I suffer from a mental health disorder, and I'm seeking help ... and other people can do the same thing."
Read the original article Here. For additional information about TMS visit Brain Wellness Center. Brain Wellness Center is located in San Ramon and Palo Alto and is one of the leading edge providers of TMS services. Each patient’s qEEG brain mapping information is utilized to customize and tailor make the treatment to their specific and unique brain pattern.
- Comments (8)
- Brain Circuit Involved in Inheritance of Anxiety in Rhesus Monkeys
- By Jason von Stietz
- July 17, 2015
-

Photo Credit: Getty Images Anxious parents are likely to have anxious children. This is true of rhesus monkeys as well as humans. Researchers at the University of Wisconsin, Madison utilized positron emission topography (PET) scans to study anxiety in multiple generations of rhesus monkeys. Findings indicated that the inheritance of an over-active brain circuit might set the stage for the development of anxiety or depressive disorders. The study was discussed in a recent issue of NeuroScientistNews:
In rhesus monkey families -- just as in their human cousins -- anxious parents are more likely to have anxious offspring. And a new study in an extended family of monkeys provides important insights into how the risk of developing anxiety and depression is passed from parents to children.
The study from the Department of Psychiatry and the Health Emotions Research Institute at the University of Wisconsin-Madison shows how an over-active brain circuit involving three brain areas inherited from generation to generation may set the stage for developing anxiety and depressive disorders.
The study is published online in the early edition of the Proceedings of the National Academy of Sciences. It shows that elevated activity in this prefrontal- limbic -midbrain circuit is likely involved in mediating the in-born risk for extreme anxiety, anxious temperament that can be observed in early childhood.
"Over-activity of these three brain regions are inherited brain alterations that are directly linked to the later life risk to develop anxiety and depression,'' says senior author Dr. Ned Kalin, chair of psychiatry at the UW School of Medicine and Public Health. "This is a big step in understanding the neural underpinnings of inherited anxiety and begins to give us more selective targets for treatment."
Previous research by Kalin's group has shown that anxious temperament is inherited, and explained the brain circuits involved. About half of children who show extreme anxiety go on to develop stress-related psychiatric disorders later in life.
Monkeys, like humans, can be temperamentally anxious and pass their anxiety-related genes on to the next generation.
By studying nearly 600 young rhesus monkeys from a large multi-generational family, Drs. Andrew Fox, Kalin, and colleagues found that about 35 percent of variation in anxiety-like tendencies is explained by family history.
To understand which brain regions are responsible for passing anxiety from generation to generation, the authors measured anxiety-related behavior with high-resolution functional and structural brain imaging. They exposed the young monkeys to a mildly threatening situation that a child would also encounter, exposure to a stranger who does not make eye contact with the monkey. During this encounter, they used imaging methods commonly used in humans (positron emission tomography, PET) to identify brain regions in which increased metabolism predicted each individual's level of anxiety.
By closely examining how individual differences in brain function and anxiety-related behavior fall through the family tree, the authors identified brain systems responsible for the parent-to-child transmission of anxiety-related behavior. Using this "genetic correlation" approach, the authors found the neural circuit where metabolism and an early-life anxious temperament are likely to share the same genetic basis.
Interestingly, the brain circuit that was genetically correlated with individual differences in early-life anxiety involved three survival-related brain regions. These regions were located in the brain stem, the most primitive part of the brain; the amygdala, the limbic brain fear center; and the prefrontal cortex, which is responsible for higher-level reasoning and is fully developed only in humans and their primate cousins.
"Basically, we think that to a certain extent, anxiety can provide an evolutionary advantage because it helps an individual recognize and avoid danger, but when the circuits are over-active, it becomes a problem and can result in anxiety and depressive disorders," Kalin explains.
Surprisingly, these studies found that it was the function of these brain structures -- and not their size -- that was responsible for the genetic transfer of an anxious temperament. Although the search for the genetic underpinnings of anxiety have thus far been elusive, this research helps explain how genes might affect brain function and lead to extreme childhood anxiety, which greatly increases the risk to develop anxiety and depressive disorders.
"Now that we know where to look, we can develop a better understanding of the molecular alterations that give rise to anxiety-related brain function,'' Kalin says. "Our genes shape our brains to help make us who we are."
Read the original article Here
- Comments (0)
- Animal Study Sheds Light on Neurocircuitry Involved in Resiliency
- By Jason von Stietz
- July 10, 2015
-

Getty Images Why are some resilient to chronic stress and not others. Findings from a recent animal study of chronic social defeat stress sheds light on the neurocircuitry involved in vulnerability or resiliency to stress. NeuroScientistNews discussed the study in a recent article:
Humans are remarkably resilient when confronted with tremendous amounts of stress and trauma. While most people are able to maintain balanced psychological and physical functioning, some people are vulnerable, or susceptible, to the negative biological, psychological, and social consequences of stress. The biological factors underlying susceptibility are unknown and likely intersect with an individual’s ability to cope, among other factors.
Emerging evidence from animal studies suggests there are distinct cellular and molecular adaptations that occur in response to stress to either promote resiliency or lead to susceptibility. The ventral striatum (vSTR) has been identified as a key brain region for regulating depression-related behaviors following chronic stress. In a recent study, Christoffel et al. elucidated the specific inputs to the vSTR mediating susceptibility to stress in mice following chronic social defeat stress (CSDS). CSDS is a well-validated model for studying the cellular and molecular underpinnings of stress-related psychiatric diseases in rodents.
The CSDS paradigm consists of pairing an experimental C57BL/6J mouse with an aggressive, CD-1 retired breeder mouse over the course of days in a cage. After each daily pairing, these mice are housed in the same cage, only separated by a partition with holes to allow for continuous ‘psychological’ stress for the experimental mouse from sensory interaction with the aggressor mouse. Following CSDS, the experimental mice are tested in the social interaction behavioral assay to assess the degree of social avoidance (i.e., anxiety and depression related behavior). The experimental mouse is placed into an open arena with the caged aggressor mouse and the amount of time spent socially interacting is recorded. Despite experiencing the same defeat stressor, experimental mice can be separated into ‘susceptible’ or ‘resilient’ groups to study the biological mechanisms contributing to these divergent phenotypes.
The authors used complementary approaches to identify and manipulate specific excitatory, glutamatergic inputs to the vSTR that mediate stress susceptibility. Projection-based viral targeting techniques revealed increased excitatory synaptic strength from the intralaminar (ILT) to the vSTR only in susceptible mice, whereas excitatory strength of the inputs to the vSTR from the prefrontal cortex (PFC) was similar between resilient and susceptible mice, suggesting enhanced ILT-vSTR signaling is relevant for stress-induced susceptibility.
Interestingly, inhibition of the ILT presynaptic inputs to the vSTR either by chronically inhibiting calcium release using viral-mediated expression of ‘tToxins’ or acutely by physiologically relevant optogenetic inhibition prevented stress-induced susceptibility, which was accompanied by reductions in excitatory postsynaptic currents (EPSCs) and the density of immature stubby dendritic spines of vSTR medium spiny neurons (MSNs).
In contrast, chronic inhibition of PFC-vSTR pathways further decreased stress-induced social interaction times and increased the density of stubby dendritic spines in the vSTR. However, acute, rapid optogenetic inhibition of this circuit had no effect on the susceptibility phenotype, suggesting sustained inhibition may be required, or other PFC efferents are responsible for promoting normal behavioral function (i.e., resiliency).
Human imaging findings indicate reduced vSTR response to various rewarding stimuli in individuals with major depressive disorder1,2,3, which are further supported by studies using deep brain stimulation of the internal capsule (includes vSTR) to alleviate symptoms of depression4. The present findings suggest that distinct glutamatergic pathways converge on the vSTR reward circuitry to mediate stress-induced susceptibility or promote resiliency. Animal studies are beginning to shed light on how stress leads to alterations in activity of particular neural circuits that could be relevant for many psychiatric diseases.
Read the orginal article Here
- Comments (0)
- Hippocampus Smaller in People with Recurrent Depression
- By Jason von Stietz
- July 3, 2015
-
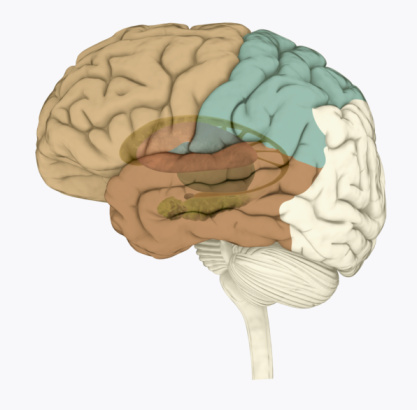
Photo Credit: Getty Images Recent research has found that the hippocampus of people with recurrent depression is significantly smaller than that of healthy individuals. Researchers from the University of Sydney examined the magnetic resonance imaging (MRI) data of nearly 9,000 participants. The findings were recently discussed in an article of Medical Xpress:
Major depression is a common condition affecting at least one in six people during their lifetime. It is a serious clinical mood disorder in which feelings of sadness, frustration, loss, or anger interfere with a person's everyday life for weeks, months or years at a time.
Key findings
The key finding that people with major depression have a smaller hippocampus confirms earlier clinical work conducted at the BMRI. In this study, the key finding was largely explained by subjects with recurrent depression. People with recurrent depression represented 65 per cent of study subjects with major depression.
People with an early age of onset of major depression (before the age of 21 years) also had a smaller hippocampus than healthy individuals, consistent with the notion that many of these young people go on to have recurrent disorders.
However, people who had a first episode of major depression (34 per cent of study subjects with major depression) did not have a smaller hippocampus than healthy individuals, indicating that the changes are due to the adverse effects of depressive illness on the brain.
Commentary
"These findings shed new light on brain structures and possible mechanisms responsible for depression," says Associate Professor Jim Lagopoulos of the University of Sydney's Brain and Mind Research Institute.
"Despite intensive research aimed at identifying brain structures linked to depression in recent decades, our understanding of what causes depression is still rudimentary.
"One reason for this has been the lack of sufficiently large studies, variability in the disease and treatments provided, and the complex interactions between clinical characteristics and brain structure."
Commenting on the clinical significance of the findings, Co-Director of the Brain and Mind Research Institute, Professor Ian Hickie says: "This large study confirms the need to treat first episodes of depression effectively, particularly in teenagers and young adults, to prevent the brain changes that accompany recurrent depression.
"This is another reason that we need to ensure that young people receive effective treatments for depression - a key goal of our Centre of Research Excellence in Optimising Early Interventions for Young People with Emerging Mood Disorder. "This new finding of smaller hippocampal volume in people with major depression may offer some support to the neurotrophic hypothesis of depression," adds Jim Lagopoulos.
"This hypothesis argues that a range of neurobiological processes such as elevated glucocorticoid levels in those with chronic depression may induce brain shrinkage.
"Clearly, there's a need for longitudinal studies that can track changes in hippocampal volume among people with depression over time, to better clarify whether hippocampal abnormalities result from prolonged duration of chronic stress, or represent a vulnerability factor for depression, or both," he said.
Read the original article Here
- Comments (0)


 Subscribe to our Feed via RSS
Subscribe to our Feed via RSS