Blog
- Amygdalar Activity Predicts Cardiovascular Events, Study Finds
- By Jason von Stietz, M.A.
- January 31, 2017
-
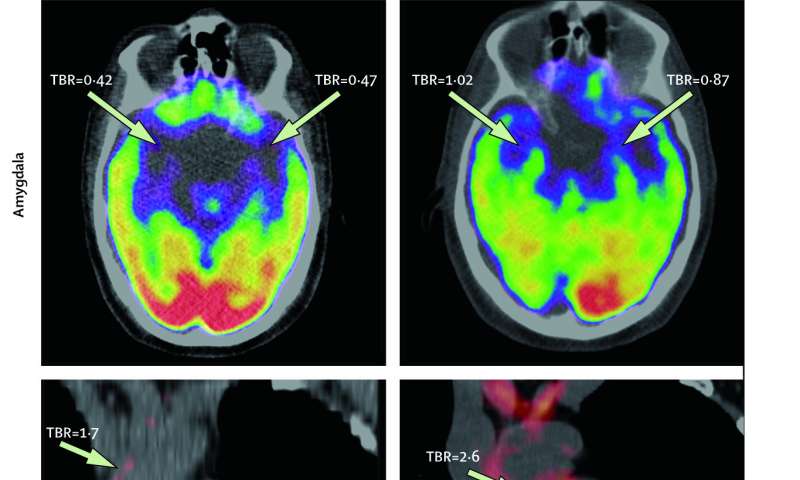
Tawakol et al, 2017, The Lancet It is well known that emotional stress is related to risk of cardiovascular disease. However, the mechanism of this phenomenon has not always been clearly understood. Researchers at Massachusetts General Hospital, Icahn School of Medicine at Mount Sinai, and Tufts University collaborated to investigate the relationship between amygdalar activity and cardiovascular events. Findings indicated that amygdalar activity predicted bone-marrow activity and arterial inflammation. The study was discussed in a recent article in Medical Xpress:
"While the link between stress and heart disease has long been established, the mechanism mediating that risk has not been clearly understood," says Ahmed Tawakol, MD, co-director of the Cardiac MR PET CT Program in the MGH Division of Cardiology and lead author of the paper. "Animal studies have shown that stress activates bone marrow to produce white blood cells, leading to arterial inflammation, and this study suggests an analogous path exists in humans. Moreover, this study identifies, for the first time in animal models or humans, the region of the brain that links stress to the risk of heart attack and stroke."
The paper reports on two complementary studies. The first, conducted at MGH, analyzed imaging and medical records data from almost 300 individuals who had PET/CT brain imaging, primarily for cancer screening, using a radiopharmaceutical called FDG that both measures the activity of areas within the brain and also reflects inflammation within arteries. All participants in that study had no active cancer or cardiovascular disease at the time of imaging and each had information in their medical records on at least three additional clinical visits in the two to five years after imaging. The second study, conducted at the Translational and Molecular Imaging Institute (TMII) at ISMMS in New York, enrolled 13 individuals with a history of post-traumatic stress disorder, who were evaluated for their current levels of perceived stress and received FDG-PET scanning to measure both amygdala activity and arterial inflammation.
Among participants in the larger, longitudinal study, 22 experienced a cardiovascular event—such as a heart attack, stroke or episodes of angina—in the follow-up period; and the prior level of activity in the amygdala strongly predicted the risk of a subsequent cardiovascular event. That association remained significant after controlling for traditional cardiovascular risk factors, and after controlling for presence of symptom-free atherosclerosis at the time of imaging. The association became even stronger when the team used a more stringent definition of cardiovascular events—major adverse cardiovascular events.
Amygdalar activity was also associated with the timing of events, as those with the highest levels of activity had events sooner than those with less extreme elevation, and greater amygdalar activity was also linked to elevated activity of the blood-cell-forming tissue in the bone marrow and spleen and to increased arterial inflammation. In the smaller study, participants' current stress levels were strongly associated with both amygdalar activity and arterial inflammation.
Co-senior author Zahi A. Fayad, PhD, vice-chair for Research in the Department of Radiology and the director of TMII at ISMMS in New York, says, "This pioneering study provides more evidence of a heart-brain connection, by elucidating a link between resting metabolic activity in the amygdala, a marker of stress, and subsequent cardiovascular events independently of established cardiovascular risk factors. We also show that amygdalar activity is related to increased associated perceived stress and to an increased vascular inflammation and hematopoeitic activity."
Tawakol adds, "These findings suggest several potential opportunities to reduce cardiovascular risk attributable to stress. It would be reasonable to advise individuals with increased risk of cardiovascular disease to consider employing stress-reduction approaches if they feel subjected to a high degree of psychosocial stress. However, large trials are still needed to confirm that stress reduction improves cardiovascular disease risk. Further, pharmacological manipulation of the amygdalar-bone marrow-arterial axis may provide new opportunities to reduce cardiovascular disease. In addition, increased stress associates with other diseases, such as cancer and inflammatory conditions, including rheumatoid arthritis and psoriasis. So it will be important to evaluate whether calming this stress mechanism produces benefits in those diseases as well."
Read the original article Here
- Comments (0)
- Weaker Connectivity In Brains of Those with Bipolar Disoder
- By Jason von Stietz, M.A.
- January 29, 2017
-

Getty Images According to the National Institute of Mental Health, 2.6 percent of the U.S. adult population suffers from bipolar disorder. Bipolar disorder is a debilitating illness that can involve several years of mental health treatment before a proper diagnosis is given. Australian researchers recently conducted a study investigating the use of MRI scans of the brain in detecting biomarkers for the disorder. Findings indicated that participants suffering from bipolar disorder had weaker connectivity in emotional centers of the brain, such as right-sided fronto-temporal and temporal areas, than their healthy counterparts. The study was discussed in a recent article in MedicalXpress:
It is hoped the findings will lead to new tools to identify and manage those at risk before the onset of the disorder and help reduce its impact once it develops.
The study, published today in the prestigious Nature journal Molecular Psychiatry, was a collaboration between researchers from QIMR Berghofer Medical Research Institute in Brisbane and UNSW in Sydney.
Researchers conducted MRI scans on the brains of three groups: people who had been diagnosed with bipolar disorder; people who had a first-degree relative (parent, sibling or child) with bipolar and who were at high genetic risk themselves; and people unaffected by bipolar disorder.
They found networks of weaker connections between different brain regions in both the bipolar and high-risk subjects and disturbances in the connections responsible for regulating emotional and cognitive processes.
"We know that changes in these brain wiring patterns will impact upon a person's capacity to perform key emotional and cognitive functions," said study author Scientia Professor Philip Mitchell from UNSW's School of Psychiatry.
"Each year we will be following up with participants from this study who are at high genetic risk of developing bipolar disorder, to see if the brain changes identified in MRI scans reveal who will develop episodes of mania," Professor Mitchell said.
Bipolar disorder is a debilitating illness affecting about one in 70 Australians. It typically involves unstable mood swings between manic 'highs' and depressive 'lows'. The age of onset is usually between 18 and 30 years.
Professor Michael Breakspear, from QIMR Berghofer and Brisbane's Metro North Hospital and Health Service, said the research team hoped to use the findings to develop a way of identifying those at risk of bipolar before the onset of the disorder.
"At the moment we don't have any markers or tests for predicting who is at risk of developing bipolar disorder, as we do for heart disease," Professor Breakspear said.
"If we can develop a tool to identify and confirm those who are at the very highest risk, then we can advise them on how to minimise their risk of developing bipolar, for example, by avoiding illicit drugs and minimising stress. These discoveries may open the door to starting people on medication before the illness, to reduce the risk of manic episodes before the first one occurs.
"Our long-term goal is to develop imaging-based diagnostic tests for bipolar. At the moment, diagnosis relies on the opinion of a doctor. Recent UNSW-led research found an average delay of six years between when a person with bipolar experiences their first manic episode and when they receive a correct diagnosis," Professor Breakspear said.
"Many people are incorrectly diagnosed with depression or other disorders. This delays the start of proper treatment with medications that are specific to bipolar disorder. Bipolar has the highest suicide rate of any mental illness, so it's crucial that we diagnose people correctly straight away so they can start receiving the right treatment."
The study was funded by the National Health and Medical Research Council and the Landsdowne Foundation.
Read the original article Here
- Comments (0)
- Underactivated Reward Center Related to Musical Anhedonia
- By Jason von Stietz, M.A.
- January 22, 2017
-

Getty Images Musical anhedonia, a condition in which individuals are unable to enjoy music, affects as much as 5% of the population. Researchers at the University of Barcelona compared the brain scans of people suffering from musical anhedonia to those of their healthy counterparts. The researchers found that those suffering from the condition showed underactivity in the nucleus accumbens, a reward center in the brain. The study was discussed in a recent article in the Worthing Herald:
Researchers found people that get little pleasure from music, who are known as musical anhedonics, show less activity in the ‘reward centre’ of the brain when songs are playing.
But musical anhedonics are able to respond to other enjoyable activities like gambling, which suggests there could be a missing link between their reward centre and the brain region which controls processing sounds.
The condition is believed to affect up to five per cent of the population.
Psychology PhD student Noelia Martínez-Molina, who led the study, said: “Although music is ubiquitous in human societies, there are some people for whom music holds no reward value despite normal perceptual ability and preserved reward-related responses in other domains.”
As part of the study at the University of Barcelona, Spain, researchers recruited 45 healthy people who completed a questionnaire measuring their level of sensitivity to music and then divided them into three groups based on their responses.
The participants were then asked to listen to music while lying inside an MRI scanner.
Scientists used the scanner to measure activity in the reward centre of the participants’ brains.They found that people who said they didn’t enjoy music showed a reduction in the activity of the nucleus accumbens, a key region in the reward centre of the brain, when songs were playing.
In contrast, people who said they liked music showed enhanced activity in the reward centre.
Researchers also analysed the brains of the music anhedonics while they were gambling to check if their reward centres could respond to other pleasurable activities.
Dr Martínez-Molina said: “We demonstrate that the music anhedonic participants showed selective reduction of activity for music in the nucleus accumbens, but normal activation levels for a monetary gambling task.”
The researchers said the fact musical anhedonics are able to respond to enjoyable activities other than music suggests there could be a missing link between the areas in their brains that control sound and pleasure.
Previous studies have shown that children on the autistic spectrum, who do not find the human voice to be pleasurable, experience a similar disconnection between the brain regions that control sound processing and pleasure.
Dr Robert Zatorre, a researcher from Montreal Neurological Institute, McGill University, Canada, who co-authored the study, said: “These findings not only help us to understand individual variability in the way the reward system functions, but also can be applied to the development of therapies for treatment of reward-related disorders, including apathy, depression, and addiction.”
The study was published in the journal Proceedings of the National Academy of Sciences.Read the original article Here
- Comments (0)


 Subscribe to our Feed via RSS
Subscribe to our Feed via RSS