Blog
- Neuroscience of Indecision
- By Jason von Stietz
- August 24, 2015
-
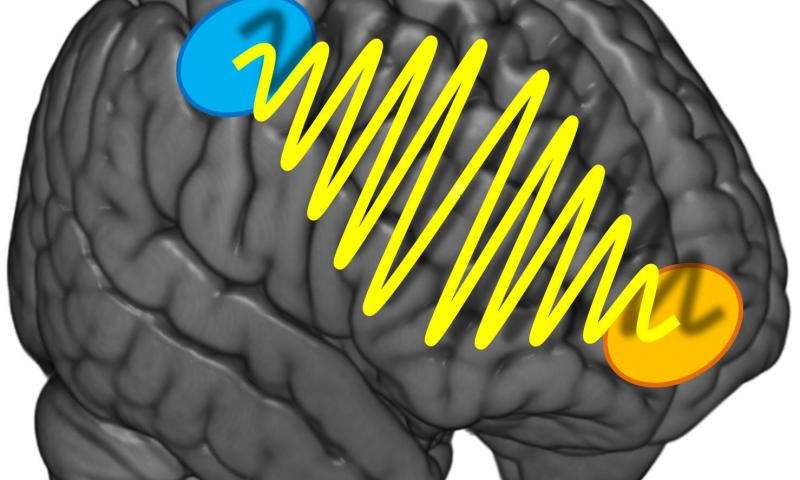
Photo Credit: University of Zurich Why is it sometimes so hard to decide what we are in the mood to eat for dinner? Should we order the steak or the veal? Researchers at the University of Zurich found that indecisiveness relates to the strength of communication between two different regions of the brain. The study was discussed in a recent article in Medical Xpress:
It's the same old story: You're in a restaurant and can't make up your mind what to order. After studying the menu for some time and many discussions, you eventually choose the steak. But you can't relax during the meal and keep wondering whether you should have gone for the veal after all. Such difficulties with decisions crop up in all aspects of life, not only food. However, they predominantly affect preference-based decisions, i.e. questions like «what do I prefer - melon or cherries?" Purely sensory decisions based on sensorial information such as «what is bigger - melon or cherry?" are less prone to indecisiveness.
The more intensive the information flow, the more decisive
How come some people are so uncertain of their preferences and keep making new choices while others know exactly what they like and want? A team headed by Professor Christian Ruff, a neuroeconomist from the University of Zurich, set about investigating this question. The Zurich researchers discovered that the precision and stability of preference decisions do not only depend on the strength of the activation of one or more brain regions. Instead, the key for stable preference choices is the intensity of the communication between two areas of the brain which represent our preferences or are involved in spatial orientation and action planning.
The researchers used transcranial alternating current stimulation, a non-invasive brain stimulation method that enables generation of coordinated oscillations in the activity of particular brain regions. The test subjects did not realize that they were being stimulated. Using this technique, the researchers intensified or reduced the information flow between the prefrontal cortex located directly below the forehead and the parietal cortex just above both ears. The test subjects had to make preference-based or purely sensory decisions about food.
«We discovered that preference-based decisions were less stable if the information flow between the two brain regions was disrupted. Our test subjects were therefore more indecisive. For the purely sensory decisions, however, there was no such effect," explains Ruff. «Consequently, thecommunication between the two brain regions is only relevant if we have to decide whether we like something and not when we make decisions based on objective facts." There was no evidence of any gender-specific effects in the experiments.
It was not possible to make the decisions more stable by intensifying the information flow. However, the study participants were young, healthy test subjects with highly developed decision-making skills. On the other hand, the results of the study could be used for therapeutic measures in the future - such as in patients who suffer from a high degree of impulsiveness and indecisiveness in the aftermath of brain disorders.
Read the original article Here
- Comments (0)
- Brain Scans Predict Success of CBT for Social Anxiety Disorder
- By Jason von Stietz
- August 20, 2015
-
.jpg)
Photo Credit: MIT News Social anxiety disorder (SAD) affects 15 million people in the United States, approximately 6.8 percent of the U.S. population. Unfortunately, many treatments of SAD succeed as often as they fail. However, researchers at MIT found that brain scans predicted which patients would benefit from CBT with an accuracy of 80 percent. Medical Xpress discussed the findings in a recent article:
For patients with social anxiety disorder (SAD), current behavioral and pharmaceutical treatments work about half the time. After weeks of investment in therapy, about half of patients will likely still suffer with symptoms of anxiety, and have little choice but to try again with something else. This trial-and-error process—inevitable due to an absence of tools to guide treatment selection—is time-consuming and expensive, and some patients eventually just give up.
But new MIT research suggests that it may be possible to do better than a coin toss when choosing psychiatric therapies for patients. The study, which performed brain scans on 38 SAD patients, found that these scans contain clues that indicate, with about 80 percent accuracy, which SAD patients will do well in cognitive behavioral therapy (CBT), an intervention designed to help patients change thinking patterns. Use of the scans to predict treatment outcomes improved predictions fivefold over use of a clinician's assessment alone.
"Choice of therapy is like a wheel of chance," says first author Susan Whitfield-Gabrieli, a research scientist in the McGovern Institute for Brain Research at MIT. "We're hoping to use brain imaging to help provide more reliable predictors of treatment response."
The researchers used a form of brain imaging that scans patients in a state of rest. Resting-state images can be done quickly, in about 15 minutes, and reliably, since they don't require patients to follow instructions, so they have the potential to be used in a clinical setting as a tool that helps doctors select the best treatments for patients.
"Knowing who to give which therapy to upfront would save time, money, and health care resources," says Greg Siegle, an associate professor of psychiatry at the University of Pittsburgh School of Medicine who was not involved in this study. "This ability would be staggering to have at our disposal for the health care system."
The findings are reported in the current issue of the journal Molecular Psychiatry. The work was carried out in the lab of principal investigator John Gabrieli, the Grover Hermann Professor of Health Sciences and Cognitive Neuroscience at MIT and a member of the McGovern Institute.
Common disorder
Social anxiety disorder affects approximately 6.8 percent of Americans, about 15 million individuals, and is the country's third-most-common mental health disorder, according to the National Institutes of Mental Health. Its symptoms include extreme anxiety in social settings that can interfere with work and quality of life. Patients living with this disorder are also at higher risk of other psychiatric disorders, such as depression and substance abuse.
The study analyzed SAD patients from the Center for Anxiety and Related Disorders at Boston University and the Center for Anxiety and Traumatic Stress at Massachusetts General Hospital. The patients were scanned prior to participation in 12 weeks of group-based CBT. They also were evaluated using a behavioral assessment tool called the Liebowitz Social Anxiety Scale (LSAS) before and after CBT to determine who had improved.
In 2013, co-author Satrajit Ghosh, a principal research scientist at the McGovern Institute, studied task-based scans of this same group of patients. He and Whitfield-Gabrieli found that scans of patients' brains as they responded to angry or neutral faces and emotional or neutral scenes predicted CBT outcomes.
"But task-based scans have downsides," Whitfield-Gabrieli says: Behavioral differences among patients can affect performance. Also, task-based scans can only be used on patients who can follow a task, which excludes infants and some elderly or very ill patients.
Scanning the resting brain
So Whitfield-Gabrieli followed this earlier research with a study of the predictive power of resting-state imaging, which she and colleagues had also performed prior to CBT. During a resting-state scan, the patient just lies there. "That's the beauty of it," she says. "They're just letting their minds wander."
Resting-state imaging provides a look at the way a patient's brain is wired, both structurally and functionally. For instance, resting-state functional magnetic resonance imaging (fMRI) shows which parts of the brain synchronize with one another during rest, suggesting that they are functionally connected. In addition, analysis of diffusion-weighted magnetic resonance imaging (dMRI) shows the underlying anatomy of the white matter tracts that interconnect distant brain regions.
Based on findings from their earlier research, Whitfield-Gabrieli and colleagues first used resting-state fMRI to look at connections to the amygdala, the seat of fear in the brain. They found that patients with higher connectivity to the amygdala from certain other regions were more likely to have lower anxiety after CBT.
They then performed a second analysis of the resting-state fMRI data, this time looking across the entire brain for patterns of connectivity. This analysis revealed additional markers that were predictive of treatment. The researchers also analyzed dMRI data and found that more robust connectivity in the tract that connects visual cues with emotional responses is also predictive of improvement with CBT.
Higher LSAS scores, which indicate more severe SAD, correlate modestly with larger improvements after CBT. In this study, each brain scan analysis had predictive value beyond the LSAS, and the three analyses together produced a fivefold improvement in predictive power over the LSAS alone.
The next step for Whitfield-Gabrieli and colleagues is to validate their predictive model on hundreds or possibly thousands of patients. Such a large-scale study may be possible because resting-state scans are comparable even when performed in different labs or by different researchers. Such comparisons weren't feasible using task-based scans, which tend to vary from lab to lab.
"Right now there's a huge movement to create massive data sets, to share resting-state imaging data, and really change the way people do science," Whitfield-Gabrieli says.
Other next steps for Whitfield-Gabrieli's group are studies to predict the success of more than one form of therapy, and to look at other psychiatric conditions, such as depression and attention disorders. "We don't want to just know if they're going to respond to one treatment," she says. "We want to know which treatment is best for each patient."
Read the original article Here
- Comments (0)
- Electrical Signals Might Facilitate the Repair of Spinal Cord Injuries
- By Jason von Stietz
- August 7, 2015
-
Researcher Li Yao. Photo Credit: Wichita State University Can the spinal cord heal itself after an injury? A researcher at Wichita State University is investigating a promising new approach that involves aiming electrical signals at the spinal cord that facilitate healing. A recent article in NeuroScientistNews discusses the new approach:
Wichita State University's Li Yao is taking a special approach to the study of spinal cord injuries through research that uses an electrical signal to repair tissue damage.
When a person suffers neurological damage to their spinal cord, the tissues surrounding the injury site can die. But one of the body's defense mechanisms is the regeneration and migration of a type of support cell -- called Schwann cells -- to the injury.
Those cells, as has been discovered in recent years, help myelinate -- or cover -- nerve axons where the injury has occurred, which promotes the recovery of some of the spinal cord's function.
Yao, a biological sciences assistant professor, is studying how electrical signals can aim those cells directly to the injury site. His research, he hopes, will open new doors for the medical field to use electrical fields in the treatment of neural injuries.
"Electrical signal is a kind of ignored approach that may generate significant biological function in neural regeneration," Yao says.
Yao's research studies the molecular mechanism of cell migration in electric fields using next-generation RNA sequencing to look at the signaling pathways that regulate cell migration.
So far, he has discovered that the precision of the cell migration toward the injury increased significantly as the strength of the electrical field increased. The electrical field did not, however, change the speed at which the cells moved.
Still, Yao's early findings suggest that the use of electrical fields in cell migration could become a burgeoning area of study in regenerative medicine.
"Our work has implications for central nervous system repair, and the application of an electrical field may assist with that," Yao says.
Read the original article Here
- Comments (0)


 Subscribe to our Feed via RSS
Subscribe to our Feed via RSS