Blog
- fMRI Neurofeedback Used to Increase Confidence and Decrease Fear
- By Jason von Stietz, M.A.
- December 31, 2016
-

What does confidence look like in the brain? Is it possible to directly train confidence? Researchers at UCLA investigated the use of fMRI neurofeedback to increase confidence and decrease fear. Researchers decoded intricate patterns of brain activity associated with confidence and fear. Neurofeedback was then used to reward the brain activity patterns, which were unconscious to the participants. The study was discussed in a recent article in MedicalXpress:
The approach, developed by a UCLA-led team of neuroscientists, is described in two new papers, published in the journals Nature Communications and Nature Human Behaviour.
Their method could have implications for treating people with depression, dementia and anxiety disorders, including post-traumatic stress disorder, said Hakwan Lau, a UCLA associate professor of psychology and the senior author of both studies. It could also play a role in improving leadership training for executives and managers.
In the Nature Human Behaviour study, the researchers showed that they could reduce the brain's manifestation of fear using a procedure called decoded neurofeedback, which involves identifying complex patterns of brain activity linked to a specific memory, and then giving feedback to the subject—for example, in the form of a reward—based on their brain activity.
The researchers tested the technique on 17 undergraduate and graduate students in Japan. Participants were seated in a functional magnetic resonance imaging, or fMRI, scanner and shown patterns of vertical lines in four colors—red, green, blue and yellow. The blue and yellow images were always shown without shocks, but the red and green patterns were often accompanied by a small electrical shock administered to their feet.
As a result, the subjects' brain patterns began to register fear for the red and green images. But the scientists learned that they could use decoded neurofeedback to lessen the subjects' fear of the red pattern. They did this by giving the subjects a small cash reward—the equivalent of about 10 cents—each time they spontaneously thought about the red lines (but gave no rewards for thinking about the green lines), which the scientists could determine in real time based on their brain activity.
The following day, researchers tested whether the participants still had a fear response to the vertical lines. The red pattern, which had been frightening because it was paired with shocks, became less so because it now was paired with a positive outcome. With the reward as part of the equation, researchers found that participants perspired much less than when they had seen the red lines previously, and their brain's fear signal, centered in the amygdala, was significantly reduced.
"After just three days of training, we saw a significant reduction of fear," Lau said. "We changed the association of the 'fear object' from negative to positive."
Participants were not told what they had to do to earn the money—only that the reward was based on their brain activity and that they should try to earn as much money as possible. And each time participants were told they had won money, their brains demonstrated more of the same pattern that had just won them the cash reward.
Although participants tried to guess which of their thoughts were triggering the rewards—some guessed humming music or thinking about a girlfriend, for example—none actually figured out how they earned the money or recognized that the researchers had effectively reduced their fear of the red lines.
"Their brain activity was completely unconscious," Lau said. "That makes sense; a lot of our brain activity is unconscious."
Participants did still register fear on their fMRI scans when they saw the green pattern because, without the financial rewards, they still primarily associated the color with shocks.
The findings could help improve upon standard behavioral therapy, in which a person who is afraid of a certain object is exposed to photos of that object, or even the object itself—which can be frightening enough that many people cannot complete treatment. Lau said using "unconscious fear reduction," like in the experiment, could be more effective in many cases.
Instilling confidence
In the Nature Communications study, which was published today, Lau and his colleagues used decoded neurofeedback to increase people's confidence levels.
Ten participants were seated in an fMRI scanner and asked to watch a computer screen with hundreds of dots moving in different directions.
Participants were asked whether the majority of dots were moving to the left or the right, and how confident they were in their responses. That initial feedback gave the researchers a chance to see how high confidence and low confidence were represented in brain patterns.
Participants then were shown dots moving in random motion and told to think about anything—and that certain thoughts would earn them cash rewards. Every time the brain pattern looked like it was representing high confidence, the participant received a reward of up to the equivalent of 10 cents; subjects received smaller rewards if their brain activity indicated less confidence.
Next, the researchers showed the students the images from the first phase of the experiment—with numerous dots primarily moving in one direction or the other. The scientists found that although students weren't any better at guessing the primary direction of the dots' motion, they had become more confident in their guesses.
By studying brain patterns, Lau said, neuroscientists can decode people's thoughts about food, love, money and many other concepts, which eventually could help them design treatments for eating disorders, gambling addiction and more. The researchers next will determine whether the techniques described in the papers can be used to help patients with real phobias.
"We are cautiously optimistic," he said.
Read the original article Here
- Comments (0)
- Neurofeedback Training of Amygdala Increases Emotional Regulation
- By Jason von Stietz, M.A.
- September 18, 2016
-

Getty Images The amygdala plays a key role in emotional regulation. Researchers from Tel-Aviv University examined the impact of neurofeedback aimed at reducing EEG activity in the amygdala on emotional regulation in healthy participants. The study was discussed in a recent article in NeuroScientistNews:
Training the brain to treat itself is a promising therapy for traumatic stress. The training uses an auditory or visual signal that corresponds to the activity of a particular brain region, called neurofeedback, which can guide people to regulate their own brain activity.
However, treating stress-related disorders requires accessing the brain's emotional hub, the amygdala, which is located deep in the brain and difficult to reach with typical neurofeedback methods. This type of activity has typically only been measured using functional magnetic resonance imaging (fMRI), which is costly and poorly accessible, limiting its clinical use.
A study published in Biological Psychiatry tested a new imaging method that provided reliable neurofeedback on the level of amygdala activity using electroencephalography (EEG), and allowed people to alter their own emotional responses through self-regulation of its activity.
"The major advancement of this new tool is the ability to use a low-cost and accessible imaging method such as EEG to depict deeply located brain activity," said both senior author Dr. Talma Hendler of Tel-Aviv University in Israel and The Sagol Brain Center at Tel Aviv Sourasky Medical Center, and first author Jackob Keynan, a PhD student in Hendler's laboratory, in an email toBiological Psychiatry.
The researchers built upon a new imaging tool they had developed in a previous study that uses EEG to measure changes in amygdala activity, indicated by its "electrical fingerprint". With the new tool, 42 participants were trained to reduce an auditory feedback corresponding to their amygdala activity using any mental strategies they found effective.
During this neurofeedback task, the participants learned to modulate their own amygdala electrical activity. This also led to improved downregulation of blood-oxygen level dependent signals of the amygdala, an indicator of regional activation measured with fMRI.
In another experiment with 40 participants, the researchers showed that learning to downregulate amygdala activity could actually improve behavioral emotion regulation. They showed this using a behavioral task invoking emotional processing in the amygdala. The findings show that with this new imaging tool, people can modify both the neural processes and behavioral manifestations of their emotions.
"We have long known that there might be ways to tune down the amygdala through biofeedback, meditation, or even the effects of placebos," said John Krystal, Editor of Biological Psychiatry. "It is an exciting idea that perhaps direct feedback on the level of activity of the amygdala can be used to help people gain control of their emotional responses."
The participants in the study were healthy, so the tool still needs to be tested in the context of real-life trauma. However, according to the authors, this new method has huge clinical implications.
The approach "holds the promise of reaching anyone anywhere," said Hendler and Keynan. The mobility and low cost of EEG contribute to its potential for a home-stationed bedside treatment for recent trauma patients or for stress resilience training for people prone to trauma.
Read the original article Here.
- Comments (2)
- fMRI Utilized in Neurofeedback
- By Jason von Stietz, M.A.
- March 25, 2016
-
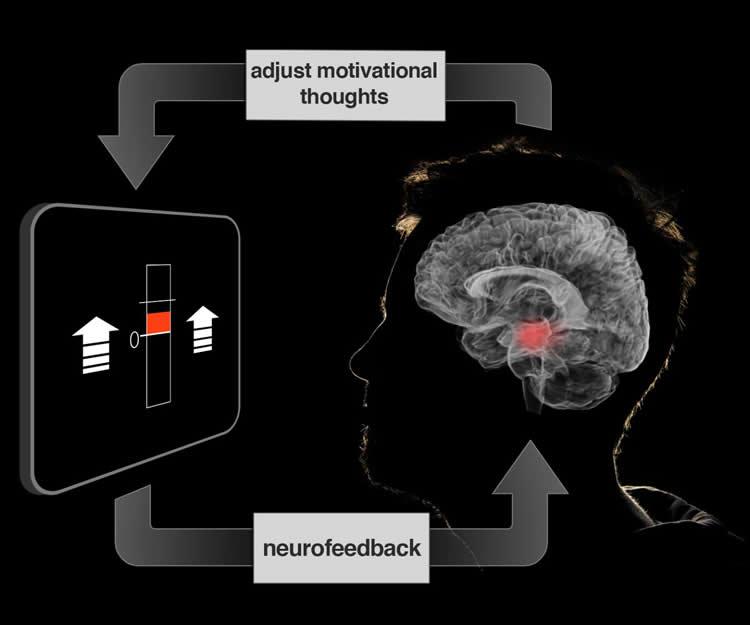
Credit: Jeff MacInnes, Duke University. Although neurofeedback has traditionally relied on the use of EEG, researchers from Duke University have examined the use of fMRI data. Participants’ brain activity was monitored and feedback was provided to them in the form of a fluctuating thermometer. Both EEG and fMRI neurofeedback were discussed in a recent article in NeuroscienceNews:
At our best, we motivate ourselves every day to get dressed and go to work or school. Although there are larger incentives at work, it’s our own volition that powers us through our innumerable daily tasks.
If we could learn to control the motivational centers of our brains that drive volition, would it lead us toward healthier, more productive lives? Using a new brain imaging strategy, Duke University scientists have now taken a first step in understanding how to manipulate specific neural circuits using thoughts and imagery.
The technique, which is described in the March 16 issue of the journal Neuron, is part of a larger approach called ‘neurofeedback,’ which gives participants a dynamic readout of brain activity, in this case from a brain area critical for motivation.
“These methods show a direct route for manipulating brain networks centrally involved in healthy brain function and daily behavior,” said the study’s senior investigator R. Alison Adcock, an assistant professor of psychiatry and behavioral sciences and associate director of the Center for Cognitive Neuroscience in the Duke University Institute for Brain Sciences.
Neurofeedback is a specialized form of biofeedback, a technique that allows people to monitor aspects of their own physiology, such as heart rate and skin temperature. It can help generate strategies to overcome anxiety and stress or to cope with other medical conditions.
Neurofeedback has historically relied on electroencephalography or EEG, in which patterns of electrical activity are monitored noninvasively by electrodes attached to the scalp. But these measures provide only rough estimates of where activity occurs in the brain.
In contrast, the new study employed functional magnetic resonance imaging (fMRI), which measures changes in blood oxygen levels, allowing more precisely localized measurements of brain activity.
Adcock’s team has been working on ways to use thoughts and behavior to tune brain function for the past eight years. In this time, they’ve developed tools allowing them to analyze complex brain imaging data in real time and to display it to participants as neurofeedback while they are in the fMRI scanner.
This study focused on the ventral tegmental area (VTA), a small area deep within the brain that is a major source of dopamine, a neurochemical well known for its role in motivation, experiencing rewards, learning, and memory.
According to Adcock’s previous research, when people are given incentives to remember specific images, an increase in VTA activation before the image appears predicts whether the participants are going to successfully remember the image.
External incentives like money work well to stimulate the VTA, but it was unclear whether people could exercise this area on their own, said co-author Jeff MacInnes, a postdoctoral researcher in Adcock’s lab.
In the new study, the team encouraged participants in the scanner to generate feelings of motivation – using their own personal strategies – during 20-second intervals. They weren’t able to raise their VTA activity consistently on their own.
But when the scientists provided participants with neurofeedback from the VTA, presented in the form of a fluctuating thermometer, participants were able to learn which strategies worked, and ultimately adopt more effective strategies. Compared to control groups, the neurofeedback-trained participants successfully elevated their VTA activity.
Participants reported using a variety of different motivational strategies, from imagining parents or coaches encouraging them, to playing out hypothetical scenarios in which their efforts were rewarded, said co-author Kathryn Dickerson, a postdoctoral researcher in Adcock’s group.
The self-generated boost in VTA activation worked even after the thermometer display was removed. Only the participants who had received accurate neurofeedback were able to consistently raise their VTA levels.
“Because this is the first demonstration of its kind, there is much still to be understood,” Adcock added. “But these tools could offer benefits for everyone, particularly those with depression or attention problems.”
The neurofeedback training also activated other regions involved in learning and experiencing rewards, confirming that, at least in the short term, the brain changes its activity more broadly as a result of neurofeedback, Dickerson said.
Adcock said one caveat of the study is that the team has not tested whether the neurofeedback drove changes in behavior. The group is working on those studies now and also plans to conduct the same study in participants with depression and attention deficit hyperactivity disorder (ADHD).
Read the original article Here
- Comments (0)
- Football Player Enhances Performance with Neurofeedback
- By Jason von Stietz, M.A.
- September 27, 2015
-

Photo Credit: Getty Images Washington Redskins quarterback Kirk Cousins has revitalized his career through not only hard work and a change in outlook but also through the use of neurofeeback training. Cousins first utilized neurofeedback during his senior year at Michigan state and again this February as he revamped his approach to his craft. Cousins new approach and experience with neurofeedback was recently discussed in an article in the Washington Post:
From the moment the Washington Redskins drafted him three rounds behindRobert Griffin III in 2012, Michigan State’s Kirk Cousins was reduced to a fallback plan. He was the football equivalent of a college applicant’s “safety school” or the friend who fills in as a prom date after true love fails.
Handed the chance to prove he could be more, Cousins stumbled last season, undercutting his 10 touchdowns passes with nine grievously timed interceptions while filling in for the injured Griffin. Even Cousins’s body language conceded defeat as he trudged off the field in Week 7, head bowed, following that ninth errant throw. He was replaced by Colt McCoy and relegated to scout-team duty the rest of the year.
Less than 11 months later, Redskins Coach Jay Gruden stepped to a microphone at Redskins Park and uttered the improbable.
“It’s Kirk’s team,” Gruden said, announcing Aug. 31 that Cousins would be the team’s starting quarterback in 2015.
Cousins hadn’t played a down in a regular season game since his benching last fall. But after a solid showing in training camp, followed by a productive preseason performance, he convinced Gruden that he represents the best hope of turning around a team with back-to-back losing seasons.
But is Cousins simply the Redskins’ best available fallback plan? Or has Cousins, at 27, learned to leverage his strengths and minimize his shortcomings after a three-year NFL apprenticeship of waiting, watching and too often short-circuiting in the limited opportunities he has had?
At first glance, little has changed about the 6-foot-3, 202-pound Cousins entering Year 4, apart from a beard that hints at a new steeliness.
Washington Redskins quarterback Kirk Cousins practiced at Estero High School near Fort Myers this winter with members of the school's varsity football team.
The overhaul of consequence, Gruden believes, is Cousins’s mental game.
His offseason work included copious film study and tutoring from a private throwing coach, as is common among NFL quarterbacks. But it included unlikely assists from a few dozen high school receivers who ran pass patterns and caught balls during Cousins’s winter vacations in Georgia and Florida and a Michigan-based company called Neurocore that Cousins said “retrained” his brain to operate in a “sweet spot” best suited to peak athletic performance.
“It’s kind of an abstract thing, but I call it brain performance,” Cousins said of his training with Neurocore Brain Performance Center, which he intensified after getting benched last fall. “I see it as the next frontier because you look at weightlifting in the 1950s and ’60s, not every football player was lifting weights; they weren’t sure about the benefit it would give you. Now everybody has a strength coach; everybody lifts weights. And I see brain training kind of being that next thing. I just want to maximize what I’ve got.”
The son of a minister and a man of deep faith, Cousins conceded that dark times followed his benching in October. The NFL career he had labored for seemed at hand after he took over for Griffin and led five touchdown drives in a 41-10 rout of Jacksonville in Week 2.
The next week, he threw for 427 yards at Philadelphia. The Redskins lost, and Cousins’s play deteriorated from there. After a 45-14 loss to the New York Giants in which he threw four second-half interceptions, Giants defenders said Cousins was telegraphing his throws.
“Anytime you have a job to do and you feel like you didn’t get the job done, it’s going to eat at you if you care about it,” Cousins said this week when asked about his mind-set after his Oct. 19 benching. “For me, I deeply care about it, and so it was eating at me.”
The turning point came, Cousins said, when he quit berating himself.
“What do I do now?” he asked himself. “What can I do to get better and deliberately practice, whatever that is.”
Once Griffin was back in the starting job and McCoy named the No. 2 quarterback, Cousins was ruled inactive. With no need to prepare for the upcoming opponent, he devoted his film-study to poring over footage of the NFL’s better quarterbacks and taking a hard look at his own footage.
When February came, Cousins and his wife, Julie, traveled to Florida’s Gulf Coast for vacation. But he wanted to keep working on his game, so he phoned a local high school near Fort Myers. He introduced himself, explained that he had his cleats and a couple footballs with him and asked whether the football coach could round up some receivers to throw to and let them use the Estero High field for a workout.
Cousins’s throwing coach, former NFL quarterback Jeff Christensen, flew in from Chicago to supervise. And for three days, Cousins threw to teenagers.
“He was dead on every time,” Estero Coach Jeff Hanlon recalled in a phone interview. “There was never a bad throw. Sometimes there was something he wasn’t happy with — maybe the height on the ball — and he wanted to adjust it. . . .
“And with every throw, he said something encouraging to the kids. Even if it was a dropped pass, he’d say, ‘Hey, great route!’ Whatever it was, he found something positive in every single rep that gave that motivation and encouragement to the kids.”
While in Florida, Cousins, joined by Redskins running back Alfred Morris, also worked with Gruden’s brother, Super Bowl champion coach turned ESPN analyst Jon Gruden, who mentors young quarterbacks in the offseason.
And while in Atlanta visiting his wife’s family, he also tracked down high school receivers to throw to.
Also in February, he ramped up his training with Neurocore, which he had begun his senior season at Michigan State.
Neurocore was founded roughly 10 years ago to help children with attention-deficit disorders through “neurofeedback” rather than medication and expanded to applications for people with sleep and anxiety disorders as well as elite athletes. Its brain-training system starts with electroencephalograms to measure the electrical activity in the brain. If the data suggests the brain is running faster or slower than is ideal, conditioning exercises are developed to help train the brain to run at what Tim Royer, the company’s founder, describes as “a sweet spot.”
According to Royer, Cousins’s data revealed that his brain was running faster than it should, relying on adrenaline much of the time. Readings of his cardiovascular system and respiratory system suggested a similar, over-stimulated condition that Royer likened to “somebody running from a lion.”
“When you try to play sports at an elite level and the body and brain are doing that, it makes it difficult over time,” Royer said in a telephone interview.
So he devised a training system to help Cousins regulate that speed and outfitted the quarterback with home-based gear to practice the exercises on his own.
In one such exercise, Cousins attaches the EEG leads to his scalp and connects it to a computer that displays the speed of his brain, heart and breathing as if it’s the dashboard of a car. Then comes the “reward system” that affirms when he has relaxed or conditioned his brain to operate in the sweet spot.
As Royer explains it, Cousins puts a movie in the computer, and a program driven by the electrical activity in the brain will play the movie only when the reading confirms that his brain is running in the optimum range.
In the early going, Royer said, Cousins might have been able to watch “Iron Man” for 20 seconds of a one-minute exercise. With practice, that period of time — time in which the brain is operated at an optimal speed — increased to 30 seconds, then 40.
On Sunday against Miami, Cousins will find himself staring at Iron Men of a different sort — lined up across from a Dolphins defensive line that Hall of Fame quarterback Dan Fouts believes is the best in the NFL.
“It’s a great opportunity for Cousins and an unbelievable challenge with that Dolphins front four,” said Fouts, who will provide commentary for the CBS broadcast. “He has to start fast and have success right away.”
Pro Bowl left tackle Trent Williams will protect Cousins’s blind side. But rookie Brandon Scherff and second-year player Morgan Moses must fend off the heart of Miami’s pass rush, sack-specialists Ndamukong Suh and Cameron Wake.
Cousins has the quickest release of the Redskins’ trio of quarterbacks, which should help. He also understands protections, Dolphins Coach Joe Philbin noted, able to bark out last-second adjustments. And he knows there’s no need for high-risk heroics after he makes a mistake, whether interception, fumble or sack.
Noting the gifted receiving and running back corps around him, Cousins said this week: “It’s my job to get them the football, then let them go do the jaw-dropping stuff.”
If boos rain down from a restive fan base, Cousins has heard them before. If he falls short of his own expectation, he has been there.
This year, if the offseason lessons stick, Cousins will take a deep breath. He will acknowledge to himself that, yes, it is a huge game, but he won’t let the magnitude paralyze him or send him into panic mode.
He will breathe deeply, settle his mind and call the next play.
Read the original article Here
- Comments (0)
- Is Neurofeedback Effective? The Washington Post Reviews Clinical Work, Research, and Personal Experiences
- By Jason von Stietz
- January 30, 2015
-

Photo Credit: Washington Post The media shined a light on the neurofeedback field in a recent article in the Washington Post. Many clinicians have developed expertise treating a variety of psychiatric disorders. Some researchers are unsure there is enough evidence to support the claims of neurofeedback practitioners. However, leading neurofeedback researchers point to the field’s recent studies as evidence. Arlene Karadis discussed the clinical work and research of neurofeedback experts and the personal experiences of their patients in a recent article:
In September 2013, Chris Gardner went from kicking and spinning as a black belt in taekwondo to being locked in a world where he could not follow conversations — or even walk his dog. The 58-year-old Vienna, Va., resident had just had brain surgery to remove a large tumor, and the operation affected his mobility and cognition.
After nine months of physical and occupational therapy, he’d made little progress. So he tried neurofeedback, hoping this controversial treatment would improve his balance and mental processes.
Neurofeedback — a type of biofeedback — uses movies, video games, computers and other tools to help individuals regulate their brain waves. A patient might watch a movie, for example, while hooked to sensors that send data to a computer. A therapist, following the brain activity on a monitor, programs the computer to stop the movie if an abnormal number of fast or slow brain waves is detected or if the brain waves are erratic, moving rapidly from fast to slow waves.
The stop-and-start feedback, repeated over and over in numerous sessions, seems to yield more-normal brain waves. Researchers who endorse the technique say they don’t know exactly how it works but they say the changes in brain waves result in improved ability to focus and relax.
Neurofeedback, which is also used for post-traumatic stress disorder and attention-deficit hyperactivity disorder, has been around since the 1960s. Some research has found it promising. Other studies have been inconclusive, and some have shown no positive outcomes.
The most solid data concern ADHD, especially a recent trial involving 104 children published in March in the Journal of Pediatrics. Those who received neurofeedback had improvements in attention and impulse control, while those who did not receive the therapy did not. These improvements persisted after six months. The authors concluded that neurofeedback may be a “promising attention training treatment for children with ADHD.”
Gardner had read that the technique could aid in recovery from brain injuries.
“I was skeptical. But I was desperate. I felt like I was wrapped in miles of cotton and could not reach through it to touch or feel anything,” said Gardner, an electronic technology consultant. His doctor was projecting a two-to-three-year recovery period, based on Gardner’s slow progress nine months after surgery.
By his ninth neurofeedback session, he was driving, taking power walks and working from home.
Neurofeedback treatments vary. In Gardner’s case, he sat in a chair while tiny, pulsed signals were sent to his brain. Research suggests that these signals enable the brain to revive its communication channels, which can become impaired after a brain injury.
“I couldn’t feel anything” while the treatments were underway, Gardner said. “I just sat there with my eyes closed. My therapist explained that the pulses basically reboot the brain.”
Better focus and relaxation can seemingly help improve or eliminate such conditions as migraines (imbalanced brain waves are associated with certain symptoms like pain) and anxiety.
He has just completed the last of 10 treatments. “I am not 100 percent. I probably won’t stand on my head or get on a roller coaster. But I can do almost everything I couldn’t do before,” said Gardner, who’s back to his martial arts.
“Do most people become totally normal? No. But they improve,” said Michael Sitar, a Bethesda psychologist certified in neurofeedback. He uses it to treat depression, ADHD, chronic pain and some other conditions.
“I find [that] people with focus problems can switch tasks easier. Kids who repeat themselves and who are emotionally labile become calmer and don’t repeat as much,” Sitar said. “With some complicated cases, like bipolar disorder, people may get by on less medication. Though less common, there are documented cases of nonverbal people who become verbal.”
Like riding a bike
Deborah Stokes, an Alexandria psychologist, compares neurofeedback to riding a bike: It’s non-conscious learning, based on the feedback, that, with repetition, can be long-lasting, she said.
“We don’t know exactly how neurofeedback works,” she said. “It’s a process where if clients get out of their own way, they relax. Over time, they get the desired brain pattern, feel calm and function better. This encourages them to stay with it.” Her team sees 30 patients a week.
Thomas Nicklin, whose family was living in Alexandria, saw Stokes for debilitating migraines. A year and a half after beginning a drug regimen prescribed by a neurologist, he was not getting better.
Nicklin, a teenager who was in boarding school, did 45 neurofeedback sessions over three months last year.
“Over time, Thomas went from three or four blinding migraines a week, vomiting and daily pain, to no symptoms,” said his mother, Pat Nicklin.
Silver Spring psychologist Robb Mapou is among the skeptics.
“I have not seen enough well-controlled, rigorous studies in most conditions for which it is recommended to show, definitively, that neurofeedback is effective. I also think there are other therapeutic factors that can contribute to an individual’s outcome, such as discussing their problems with a therapist.”
Michelle Harris-Love, a neuroscience researcher at the MedStar National Rehabilitation Network in Washington, agrees.
“I believe it is applied in some situations where we do not have enough information on the cause of a disorder or how recovery happens,” she said.
But Rex Cannon, past president of the International Society for Neurofeedback and Research, based in McLean, Va., cited nearly 200 peer-reviewed published articles that indicate neurofeedback’s effectiveness. This includes a meta-analysis of 10 studies on epilepsy patients: Although they had not responded to medications, they had a significant reduction in seizures after neurofeedback treatment. And a study on migraine patientsreported, “Neurofeedback appears to be dramatically effective in abolishing or significantly reducing migraine frequency in the great majority of patients.”
Patients usually have sessions two or three times a week, for a total of 10 to 40. Most sessions are 30 to 60 minutes long. They can be expensive — from $50 to $130 each. Some insurance policies cover neurofeedback, depending on the diagnosis.
Practitioners who use neurofeedback for medical and psychological disorders must have health-care degrees and are regulated by state agencies.
About 1,850 professionals have been certified through the Biofeedback Certification International Alliance. To earn that credential, they must undergo 36 hours of study in neurophysiology and related topics, complete a mentoring program to learn clinical skills and pass a standardized exam.
Mary Lee Esty, a Bethesda clinical social worker, has a small study underway treating veterans with PTSD. In an earlier study of seven veteranswho used neurofeedback, she reported, the results were promising.
“These people [in the early study] initially had minimal function. They could not work, and many attempted suicide,” she said. “One is getting a PhD now. One has a full scholarship when he could not read after his head injury. All of them are doing well.”
Other studies describe results of the therapy in a similar way, as promising but requiring further examination.
Esty, who received a National Institutes of Health grant for an earlier study of brain-injured patients, has used neurofeedback to treat more than 2,500 people, mainly with brain injuries or PTSD. In her most recent and still ongoing study, she collaborates with the Uniformed Services University of the Health Sciences, which gives participants in her program post-treatment evaluations.
“I am in this collaboration because I want to get the hard data out there,” Esty said.
Read the original article Here
- Comments (2)
- Neurofeedback to Help Survivors of Sexual Assault
- By Jason von Stietz
- August 22, 2014
-

Photo Credit: Daily Press Lanny Fly, family therapist and neurofeedback practictioner, plans to use neurofeedback to help survivors of sexual abuse and sexual slavery in the Congo. In the Congo and nearby areas sexual assault is commonly used as an instrument of war, which has long lasting implications to the physical and mental health of the survivors. Fly plans to help the survivors by using neurofeedback to calm their highly active amygdalas. The Daily Press discussed Fly's mission and the issue of sexual assault in a recent article:
"All feeling memories are mediated through a part of the brain called the amygdala and it doesn't go through the logical part of the brain at all," Fly said. "So we're calming that down, helping them separate the feelings from the event so when something triggers memories of the event they no longer have the powerful feelings that took over – they're able to engage their rational mind."
Fly, who's been using neurofeedback at his Newport News practice Fly Family Therapy and Neurotherapy for 15 years, believes that he got a message from God to take his skills to the Congo. He's preparing to travel with a team of five to the Bukavu in eastern Congo, an area deemed "the rape capital of the world" by the United Nations. They will work with a local hospital, teaching medical professionals how to use neurofeedback with other types of therapy to aid sexual assault victims.
"They will be very thankful... They're very thankful about anything, and this is huge. This is a life changer, you know?" Hearing said.
Sexual slavery and rape affect women both physically and mentally. During the assaults many women undergo genital mutilation or catch sexually transmitted diseases so Panzi, the Bukavu hospital, has partnered with the nearby Church of the Holy Spirit. While the hospital works to restore the women's bodies, the church helps them with social skills and provides small business seed money.
"For the Congo and that part of Africa, rape is an instrument of war and trying to intimidate people," Fly said. "It has nothing to do with sex. It's a brutal type thing. It's always mutilation involved, too... They have men who they know have HIV and have them come in and do a lot of the raping."
Fly's son David, who works with his father, added, "These are women that after they have been essentially in sexual slavery for a period of time and watched their families murdered in front of them, they have been rejected by their villages back home as being unclean. They have nowhere to go so the church has taken them in, in conjunction with the hospital, to give them a new life."
Hearing grew up in Goma, a city close to Bukavu, and has extended family who suffered sexually during the war. In 1997 as new president Laurent Desire Kabila took power, rebel soldiers with guns came into her uncle's house seeking to rape his wife. The left Hearing's aunt alone and instead stole the couple's television set, but the experience was enough to send the family running for their lives.
"Their [the soldiers] mentality was just to hurt people, to just humiliate people. To have control over people," Hearing said. "I ran for my life... We had to evacuate. We literally were living outside for a month. Outside in a tent. It would pour rain. We just had a little blanket over us. I remember like it was yesterday – a little blanket on top of your head."
Hearing believes that adding neurofeedback to the existing efforts of the hospital and church will give Congolese women an opportunity to restore their sense of self-worth and normalcy.
"I think it's going to change who they are, because women are raped there every day... It's something that will change their brain but it's also going to change their lives," she said.
Hearing attributes the brutal warfare to bad leadership and isolation from the Kinshasa, the capital.
"Everybody wants a piece of land, everybody wants a piece of the goods, the riches. Everybody wants to be in power," she said. "I am very humbled to be able to help my own people, where I'm from... I count my blessings every single day. I wake up, I'm alive, I'm breathing and I just say, 'Wow, I'm in this country...' It's a privilege."
Read the Full Article Here
- Comments (0)
- Pentagon's Brain-Powered Video Games Might Treat PTSD
- By Jason von Stietz
- July 8, 2014
-

Photo Credit: US Marine Corp/Flickr Could neurofeedback effectively treat PTSD in veterans or is the reductions of symptoms the result of the placebo effect? Researchers at the Naval Academy in San Diego announced plans for an upcoming clinical trial comparing neurofeedback treatment to a sham controlled procedure in a sample of 80 patients. Wired discussed the study in a recent article:
“When the brain sees itself interacting with the world, it becomes interested in that,” Dr. Siegfried Othmer, chief scientist at LA’s EEG Institute and responsible, along with his neurobiologist wife Sue, for “The Othmer Method” — a specific approach to neurofeedback being used in the military trial — told me last year. ”Likewise, when it sees the signal on-screen and realizes it’s in charge, it becomes interested. You might not notice, but the brain takes notice.”
The realm of brain plasticity is relatively new, but neurofeedback actually isn’t. The procedure first gained notoriety in the 1960s as a treatment for everything from migraine headaches to bed-wetting. Still, in part because of a paucity of mainstream scientific research, the approach has long been relegated to the realm of bunk science. “I think the practice has gotten ahead of the science,” Dr. Andrew Leuchter, a professor at UCLA’s Semel Institute for Neuroscience and Human Behavior, told me. “It wouldn’t be surprising … if much of the benefit was attributable to the placebo response.”
Despite such mainstream skepticism, neurofeedback is already being used by several military doctors and psychologists. Maj. Michael Villaneuva — nicknamed “The Wizard” by his patients — has performed NF on several hundred active-duty soldiers, and even brought his game console and electrodes on a deployment to Afghanistan this year. And Dr. Jerry Wesch, who leads a PTSD recovery program at Fort Hood, describes the results of his own neurofeedback trials on patients as “jaw dropping.”
Upwards of a thousand former soldiers have also tried neurofeedback, thanks toHomecoming 4 Veterans, a non-profit started by the Othmers that offers free NF to veterans through a network of 200 practitioners nationwide. The two are also responsible for training Villaneuva and other military docs in the art of NF.
Already, the Othmers are confident that the military’s clinical trial, expected to kick off in December, will yield positive results. And they hope that the trial, once complete, lends more credence to the therapy they’ve helped pioneer. “I think the trial could be huge, not only with [medical] academia, but for clinicians,” Sue tells Danger Room. “They’re often wary of adapting procedures that haven’t seen evidence-based study. So this checks off an important box.”
But the trial won’t be easy: Controlled tests of processes, rather than pharmaceuticals, are notoriously tough. That’s because designing and executing a “sham” procedure is much more difficult than, say, just doling out sugar pills instead of the real drug.
Then again, for soldiers who credit neurofeedback with their recovery from PTSD, the execution or academic impact of a clinical trial is hardly the most important thing. “How it works doesn’t matter to me,” Staff Sgt. Justin Roberts, who underwent the process at Fort Hood, told me. “Just as long as it does.”
Read the Full Article Here
- Comments (0)
- Neurofeedback Increases Affection, Builds Empathy
- By Jason von Stietz
- June 17, 2014
-
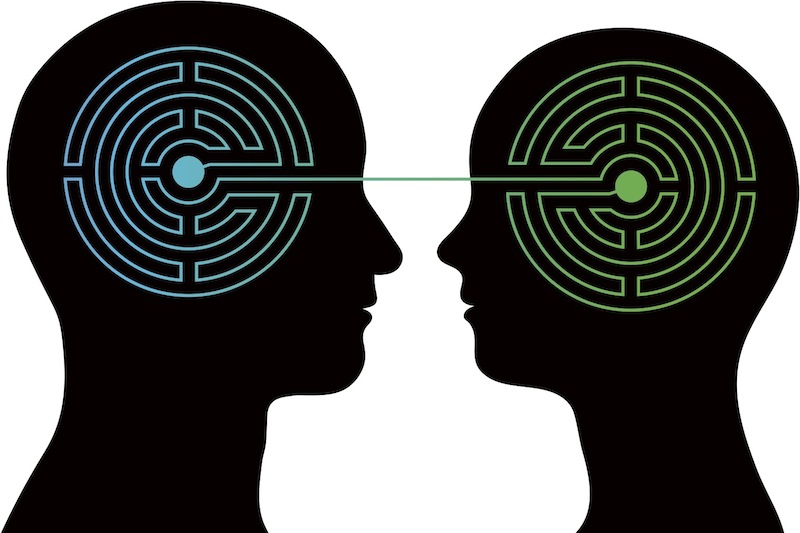
Photo Credit: Shutterstock Could neurofeedback improve "tenderness" or empathy? Researchers from the D’Or Institute for Research and Education (IDOR) and the Federal University of Rio de Janeiro investigated the impact of fMRI neurofeedback on affiliative emotion. They found that, compared to a control group, participants who underwent fMRI neurofeedback showed significantly greater brain activity related to affiliative emotion. It is possible that these findings could enhance compassion, assist couples' to resolve conflicts, and even enhance empathy in individuals with social issues or even more sever personality disorders. Scientific American discussed the study in a recent article:
The research group, led by IDOR cognitive neuroscientist Jorge Moll, focused on brain activity associated with affiliative emotions, or the warm and fuzzy—but not romantic—sensation one experiences when seeing a beloved friend or family member. To contrast this feeling with other emotional states, the researchers first asked their 24 volunteers to prepare three personal anecdotes: a proud moment, an episode full of affectionate feelings and a neutral but social scenario such as supermarket shopping. Pride and tenderness are complex social emotions, and so the researchers reasoned that comparing results from these two, along with a neutral control, could help clarify what brain activity was associated with affiliative emotion specifically.
Next, subjects had to recall these occasions while lying in a functional magnetic resonance imaging (fMRI) chamber and viewing a screen that showed a circle that would ripple and change shape. For half the subjects, the circle reflected ongoing changes in brain activity. The other half saw a randomly morphing ring described as a focal point for their visual attention. During a series of trials the researchers repeatedly cued participants with the words “proud,” “neutral” or “tender” and instructed them to relive the related memory in as much detail and emotional intensity as possible.
The researchers contrasted the data from tender, neutral and proud responses across trials to identify brain activity most related to affiliative feelings for each subject. They then assessed how much the brain response in each trial resembled this typical affiliative activity. The group given random visual feedback showed no significant difference in affiliative activity over trials. By contrast, subjects who received neurofeedback showed significantly stronger affiliative brain activity in their last trials compared with their first ones. In other words, something about seeing their brain’s changes intensified that response over subsequent trials.
To better contextualize their results, Moll and colleagues also analyzed the relevant brain regions for tender feelings across subjects. As they report in PLoS ONE on May 21, the brain regions involved included the frontopolar and septohypothalamic areas, both linked previously to affectionate feelings in earlier research.
The findings, suggests University of California, San Diego, cognitive scientist Jaime Pineda, are fairly convincing. The study is “very interesting and consistent with other fMRI neurofeedback results,” he says.Read the full article Here
- Comments (0)
- "Better Treatment, Prevention of Concussions Underway" "ABC7 News"
- By Jason von Stietz
- June 2, 2014
-
According to ABC7, News High Performance Neurofeedback (HPN) is currently used to treat veterans with PTSD and brain injuries. HPN Neurologic is conducting nationwide clinical trials are now underway examining the use of HPN for the treatment of brain injuries in the treatment of retired NFL players.
Retired NFL player Kenny Greene, who played safety for the St. Louis Cardinals, spoke to ABC7 News. Greene stated, “there’s a huge population of guys that have had injury, brain trauma, that are dealing with the consequences.” Football is a rigorous and contact sport. In spite of protective gear, such as a helmet and pads, injuries are often an inevitable part of the sport.
Joe Odom, who played linebacker for the Buffalo Bills, is one of many retired NFL players who suffers the consequences of football related brain injuries. Fortunately, Odom has found neurofeedback to be an effective treatment. Odom told ABC7 News that HPN was “he only thing that has consistently and immediately relieved a lot of the issues.”
Co-Investigator of the HPN nationwide clinical trials, George Rozelle, was quoted by ABC7 News as saying, “Up until now we have been very limited with what we can do with post concussive injuries. And this type of neurofeedback system can be applied to all forms of head injury. From kids playing youth sports to pro athletes and veterans suffering from blast injuries.”
HPN clinical trials involve the use of blood testing, extensive baseline testing, a complete neurological exam, qEEG, and Diffusion MRI. For more information about HPN Neurologic and their nationwide study Click Here
- Comments (0)
- Learning How to Listen with Neurofeedback
- By Jason von Stietz
- March 9, 2014
-
When listening to music or learning a new language, auditory perceptual learning occurs: a process in which your recognition of specific sounds improves, making you more efficient in processing and interpreting them. Neuroscientist Alex Brandmeyer shows that auditory perceptual learning can be facilitated using neurofeedback, helping to focus on the sound differences that really matter.
Read the Full Article Here
.jpeg)
Study Participant Connected to the EEG Equipment - Comments (0)


 Subscribe to our Feed via RSS
Subscribe to our Feed via RSS