Blog
- fMRI and EEG Study of Decision-Making Processes in Brain
- By Jason von Stietz, M.A.
- September 19, 2015
-

Photo Credit: Getty Images Researchers at the Institute for Neuroscience and Psychology at the University of Glasgow investigated the processes in the brain related to learning to avoid making mistakes and learning to make god decisions. The study simultaneously utilized EEG and fMRI allowing researchers to study decision-making in the brain with both the high temporal precision offered by EEG and the ability to detect precisely where these process are taking place in the brain offered by fMRI. The study was discussed in Neuroscience News:
Imagine picking wild berries in a forest when suddenly a swarm of bees flies out from behind a bush. In a split second, your motor system has already reacted to flee the swarm. This automatic response – acting before thinking – constitutes a powerful survival mechanism to avoid imminent danger.
In turn, a separate, more deliberate process of learning to avoid similar situations in the future will also occur, rendering future berry-picking attempts unappealing. This more deliberate, “thinking” process will assist in re-evaluating an outcome and adjusting how rewarding similar choices will be in the future.
“To date the biological validity and neural underpinnings of these separate value systems remain unclear,” said Dr Marios Philiastides, who led the work published in the journalNature Communications.
In order to understand the neuronal basis of these systems, Dr. Philiastides’ team devised a novel state-of-the-art brain imaging procedure.
Specifically, they hooked up volunteers to an EEG machine (to measure brain electrical activity) while they were concurrently being scanned in an MRI machine.
An EEG machine records brain activity with high temporal precision (“when” things are happening in the brain) while functional MRI provides information on the location of this activity (“where” things are happening in the brain). To date, “when” and “where” questions have largely been studied separately, using each technique in isolation.
Dr. Philiastides’ lab is among the pioneering groups that have successfully combined the two techniques to simultaneously provide answers to both questions.
The ability to use EEG, which detects tiny electrical signals on the scalp, in an MRI machine, which generates large electromagnetic interference, hinges largely on the team’s ability to remove the ‘noise’ produced by the scanner.
During these measurements participants were shown a series of pairs of symbols and asked to choose the one they believed was more profitable (the one which earned them more points).
They performed this task through trial and error by using the outcome of each choice as a learning signal to guide later decisions. Picking the correct symbol rewarded them with points and increased the sum of money paid to them for taking part in the study while the other symbol did not.
To make the learning process more challenging and to keep participants engaged with the task, there was a probability that on 30% of occasions even the correct symbol would incur a penalty.
The results showed two separate (in time and space) but interacting value systems associated with reward-guided learning in the human brain.
The data suggests that an early system responds preferentially to negative outcomes only in order to initiate a fast automatic alertness response. Only after this initial response, a slower system takes over to either promote avoidance or approach learning, following negative and positive outcomes, respectively.
Critically, when negative outcomes occur, the early system down-regulates the late system so that the brain can learn to avoid repeating the same mistake and to readjust how rewarding similar choices would “feel” in the future.
The presence of these separate value systems suggests that different neurotransmitter pathways might modulate each system and facilitate their interaction, said Elsa Fouragnan, the first author of the paper.
Dr Philiastides added: “Our research opens up new avenues for the investigation of the neural system underlying normal as well as maladaptive decision making in humans. Crucially, their findings have the potential to offer an improved understanding of how everyday responses to rewarding or stressful events can affect our capacity to make optimal decisions. In addition, the work can facilitate the study of how mental disorders associated with impairments in engaging with aversive outcomes (such as chronic stress, obsessive-compulsive disorder, post-traumatic disorder and depression), affect learning and strategic planning.
Read the original article Here
- Comments (0)
- Neuropsychoanalysis: An Emerging Field
- By Jason von Stietz
- September 12, 2015
-
Getty Images There is a new burgeoning field that combines two, often considered fundamentally different fields, neuroscience and psychoanalysis: neuropsychoanalysis. Although collaboration between these schools of thought seem surprising to many, it appeared obvious to Mark Solms, the pioneer of neuropsychoanalysis. This interesting new field was discussed in a recent article in The Atlantic:
I am in an apartment on the Upper East Side of Manhattan, surrounded by psychoanalysts. At moments, if I half close my eyes, I can imagine I’m in some European city, circa 1930: “The Kleinians have this very disturbing, I think, notion of countertransference as being something the patient does to you. They’re moving too far away from Freud’s understanding…” But in fact it’s 2010, and the conversation is new.
The experience of sitting on the edge of the huddle of analysts is, I imagine, like reading Dickens in the original serial: ongoing storylines, full of vivid characters, perpetually left in suspense. One analyst describes her work with Theo, a 30-year-old left in a wheelchair with global brain damage after a car accident, whose mother brought him to analysis with severe mental impairments and memory problems. Another discusses the progress he has made with Harry, left aphasic after a stroke, still able to comprehend but unable to express language.
Mark Solms, the neuropsychologist and psychoanalyst who founded this group in 2001, and continues to oversee its progress, is hardly the first to turn to brain damage seeking insight. Many of neuroscience’s greatest and most legendary discoveries have tumbled forth from damaged brains—from Phineas Gage, the 19th-century railroad worker whose frontal-lobe injury illuminated the brain mechanisms of self-control, to the patient known as H.M., whose radical surgery provided scientists with the ultimate test case for how the brain organizes memory.
But instead of waiting for these case studies to turn up, Solms decided to seek them out himself, and to see what might come from applying to their injuries an unorthodox means of investigation. Solms has spent his career bringing Freudian theory into the room where only biological fact had previously existed. He is a leading figure in a new interdisciplinary undertaking—along with a growing number of analysts, scientists, and others—named neuropsychoanalysis.
In the popular imagination, the term “psychoanalysis” conjures up silent doctors in dimly lit rooms, witnesses to the unfurling of dream images and childhood memories. And couches, lots of couches. This is the stereotype, the myth, but the field wielded an enormous authority throughout the 20th century, and continues to influence our most basic assumptions about human nature, like the power of the unconscious mind, the profound importance of early childhood experience, and the fact that memory is fundamentally dynamic.
Psychoanalysis has since taken on the aspect of the underdog. Many—maybe most—are unwilling to call the study of inner reality, psychic conflicts, dynamic forces and repressed material a science. And until recently, there has been relatively little empirical proof that psychoanalysis even works. Up against the quick and easy fixes of prescription medication or short-term, practically oriented cognitive-behavioral therapy—and under the skeptical eye of insurance companies—psychoanalysis faces an uncertain future.
Today, neuroscience is the golden child, commanding newspaper headlines, substantial government grants, and an ever-increasing portion of the public imagination. With its armament of modern tools and acronyms, it offers a seemingly endless list of options for looking at the brain. Neuroscientific findings are morphing into cultural truths: We are “hardwired,” a collection of parts, of “circuits” and “networks” that “light up” when “activated.” The brain has become our modern metaphor; it is where we look to find out what’s really going on. Already, neuroscientific research has penetrated the field of economics, the courts, and beyond. It is decidedly less common to hear psychoanalytic concepts invoked in these same circles.
With their starkly different goals, methods, and cultures, psychoanalysis and neuroscience can appear to be two different species, mutually alienated, as if preoccupied with two altogether different pursuits. But to some, like Solms, they are merely two views of the same object. Psychoanalysis looks at the brain from the inside out: What does it feel like to be this thing? Neuroscience looks at the brain from the outside in, measuring its behavior, investigating its physical mechanisms.
Solms supervises the progress of his group of New York psychoanalysts on monthly trips from South Africa. Tall, solid, and thick-wristed, Solms is in his late forties, but looks older. His gray hair, poking up in all directions, is completely unattended to, like a member of the family with whom he is no longer on speaking terms. In New York, he listens to developments in the group’s roster of psychoanalytic cases. In Cape Town, he is a professor of neuropsychology, making rounds in the University of Cape Town’s teaching hospital, and chairing the university’s neuropsychology department. He leads a kind of double life—one that began in the early days of his career, when he worked with brain-damaged patients by day at the Royal London Hospital, training at the Institute of Psychoanalysis by night.
Solms first trained in neuropsychology—a branch of neurology that draws links between people’s external behaviors and the specific regions of the brain involved in producing them—thinking that of all the subsets of neuroscience, neuropsychology was, as he puts it, “where you’re most likely to find out about the person himself.” But he was disappointed. Neuropsychology seemed to avoid everything that had to do with questions of personality, emotion, motivation—in other words, the things we mean when we speak of “human nature.” Instead, the operating gaze was trained onto the strictly quantifiable: How many digits could the patient hold in his working memory? Neuropsychology, Solms discovered, asked black-and-white questions that could be answered on standardized tests.
“Oliver Sacks has this saying: Neuropsychology is admirable, but it excludes the psyche,” Solms says.
Solms first heard of Freud as an undergraduate, when he stumbled across a seminar in the comparative literature department. He showed up a few weeks after the start of the semester, just as the class was assigned Freud’s lesser-knownProject for a Scientific Psychology, a summary of his attempts grapple with neurology in the years before he turned his full attention to the psychological. After completing his training as a neuropsychologist, Solms began to school himself in Freud’s ideas in earnest, and when he moved to London in his late twenties, began to train as a psychoanalyst. For the past decade, in his off hours, he has been working on the revision of James Strachey’s original English translation of the complete Standard Edition of Freud, all twenty four volumes. He often wonders what he’s gotten himself into.
It took Solms some time to understand that his inclination to combine two branches of psychology would be seen by many as controversial or problematic; that the two disciplines, psychoanalysis and neuroscience, are mostly indifferent to each other, and even, at times, opposed. But for Solms, they were intuitively compatible.
“I say it was obvious to me—why wasn’t it obvious to everyone?” Solms told me. “Like everything else, it was personal. My brother was brain-injured. When he was 6, he fell off the roof and suffered a closed head injury. I saw that my brother is not who he was. His personality is different and our whole family is different. All of that because this organ is not functioning as it was before.”
Solms and his work have a magnetic pull. People uproot their lives and come to South Africa to enter into his orbit. When I visited Solms in Cape Town, there were two such examples on hand: a Swiss expert on neuropeptides and a psychoanalyst from Vienna, both of whom had both moved to Cape Town specifically to work with Solms. The latter was preparing to begin a study that Solms had designed: psychoanalyzing a population of patients with Urbach-Wiethe disease, an extremely rare genetic disorder in which a person’s amygdala gradually calcifies until it is almost completely defunct. Solms was particularly interested in what effect this might have on the content of their dreams.
“Biology is truly a land of unlimited possibilities. We may expect it to give us the most surprising information, and we cannot guess what answers it will return in a few dozen years to the questions we have put to it.”
So reflected Freud in 1920. Having spent 20 years toiling away in labs, peering down microscopes, he arrived at the conclusion that the questions he wanted to answer about the human mind couldn’t be answered by what was then understood—or understandable—about the human brain. The knowledge wasn’t there, and neither were the tools. He continued to emphasize, however, that eventually, long after his own lifetime, the moment would come when brain science would be ready to fill out the psychoanalytic principles that he was busy laying down. Solms and his followers believe that moment is here.
It can be difficult to see how someone like Solms fit into the neuroscientific landscape. To say “Freud” to scientists engaged in the pursuit of empirical truths is to risk making yourself instantly suspect and quickly irrelevant. Yet however unlikely the idea, however unimaginable the design, neuropsychoanalysis may offer something valuable: a sketch of inner life where creativity isn’t simply explained as patterns of electrical waves, sadness as the number you circle between one and nine, and love confused with the mating habits of prairie voles.
As Solms told me: “There can’t be a mind for neuroscience and a mind for psychoanalysis. There’s only one human mind.”
Read the original article Here
- Comments (0)
- The Neural Activity of Happy Older Couples
- By Jason von Stietz
- September 4, 2015
-

Photo Credit: Getty Images Does being in a long-term and committed relationship change our neural activity? Researchers at the Rotman Research Institute Toronto and University of Toronto studied the brain scans of 14 older adult women while they viewed of either their husbands or strangers. One interesting finding was that women who reported higher relationship satisfaction showed greater activation in brain regions containing mirror neurons. The study was discussed in a recent article in Slate:
Have you ever waited with excitement to share some amazingly good news with your partner, only to experience a surge of frustration and resentment when he or she barely reacts to your announcement? As a society, we place a huge amount of emphasis on being there for each other when we’re in need, but past research has actually shown that relationship satisfaction is influenced as much, if not more, by how we react to each other’s good news. Whereas emotional support from a partner when we’re down can have the unfortunate side-effect of making us feel indebted and more aware of our negative emotions, a partner’s positive reaction to our good news can magnify the benefits of that good fortune and make us feel closer to them.
Now an unusual brain-imaging study, published recently in Human Brain Mapping, has added to this picture, showing that the relationship satisfaction of longtime married elderly women is particularly related to the neural activity they show in response to their husbands’ displays of positive emotion, rather than negative emotion.
Psychologist Raluca Petrican at the Rotman Research Institute in Toronto and her colleagues at the University of Toronto recruited 14 women with an average age of 72 who’d been married for an average of 40 years. The researchers scanned these women’s brains as they watched some carefully prepared videos.
The silent ten-second videos showed each woman’s husband or a stranger displaying an emotion that mismatched the way the video clip was labeled in a one-sentence description on the screen. For example, the clip might show the husband smiling or laughing about a happy memory (such as the first house they bought), but the video was labeled misleadingly to suggest that the man was showing this emotion while talking about a sad memory (such as the time he got fired). Other videos showed the reverse mismatch: a negative emotional display, ostensibly shown while talking about the memory of a happy event.
Essentially, the videos were designed to make the women feel like they were seeing their husband or the stranger display a surprising emotional reaction that didn’t match their own feelings. The real-world equivalent would be a situation in which a husband is happy about something that his wife doesn’t “get”; and the questions are whether she will notice, and whether she is she more sensitive to this incongruent emotion in her husband than she would be in a stranger.
The first important finding to emerge from this setup was that the women showed enhanced overall brain activity—which suggests more mental and emotional neural processing —when watching the videos of their husbands compared with videos of the strangers, but only when the videos showed displays of surprisingly incongruent positive emotion. During the other types of videos (when the men appeared to display strangely negative emotion), the women’s brains showed just as much overall activity when watching a stranger as when watching their husband. In other words, their levels of whole-brain activity betrayed a special sensitivity to their husband’s (versus a stranger’s) unexpected positive emotion.
This jibes with the past research that’s shown it’s our response to our partners’ positive news that is all-important for relationship satisfaction. Remember that these women had been married for decades, so it’s likely that they and their husbands have been doing something right relationship-wise. The brain-imaging data suggest part of the reason might be that the women are acutely tuned to when their husbands are showing happiness that’s personal to them (rather than common to both partners).
This specific interpretation trips up a little with another main result: The women’s levels of marital satisfaction (according to a questionnaire) correlated with the amount of neural processing they showed in response to their husbands’ positive and negative emotion.
However, the special importance of how we respond to our partners’ positive emotion was supported by another key finding. Namely, women who scored higher on relationship satisfaction showed more brain activation in regions thought to contain mirror neurons (neurons that are considered important for empathy) when watching their spouses than they did when watching a stranger. Moreover, this enhanced mirror-neuron activity was especially present for the videos showing their husbands’ positive, rather than negative, emotion. Again, this appears to support the idea that marital happiness goes hand in hand with sensitivity to our partners’ positive emotion (though the researchers acknowledge a different or complementary interpretation that people in happy relationships have a suppressed response to their partners’ incongruent negative emotion).
We need to interpret these preliminary and complex findings with caution. And the exclusive focus on wives’ reactions to their husbands’ emotions does lend the study a slightly retro ’70s vibe—what about the way that husbands respond to their wives’ emotions, and the importance of that for the marital happiness of both parties? But that said, the results are tantalizing in suggesting that at a neural level, people in a long-term, committed relationship are especially sensitive to their partners’ positive emotion, and particularly so when this emotion is different from their own. This neatly complements other past research showing, for example, that people who are unable to differentiate their partners’ emotions from their own (they assume they’re the same), tend to be viewed by their partners as more controlling and smothering.
As a whole, this entire body of research gives pause for thought. How do you react when your partner arrives home on an emotional high? Would you only notice if you were feeling happy too?
Read the original article Here
- Comments (0)
- Neuroscience of Indecision
- By Jason von Stietz
- August 24, 2015
-
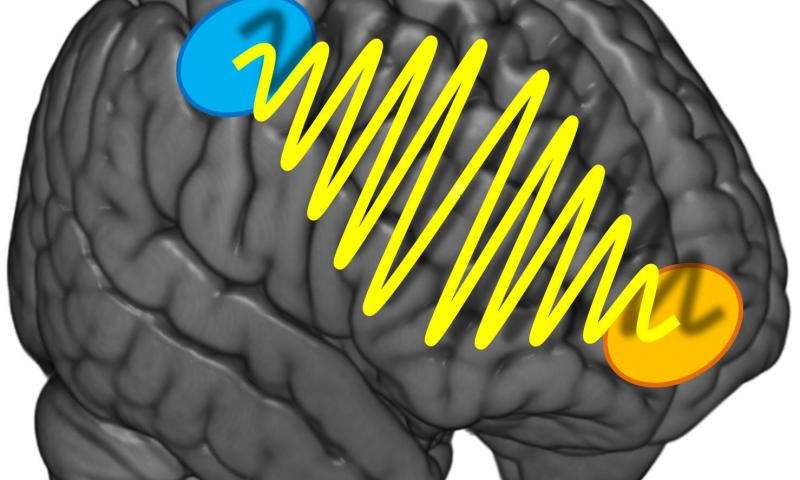
Photo Credit: University of Zurich Why is it sometimes so hard to decide what we are in the mood to eat for dinner? Should we order the steak or the veal? Researchers at the University of Zurich found that indecisiveness relates to the strength of communication between two different regions of the brain. The study was discussed in a recent article in Medical Xpress:
It's the same old story: You're in a restaurant and can't make up your mind what to order. After studying the menu for some time and many discussions, you eventually choose the steak. But you can't relax during the meal and keep wondering whether you should have gone for the veal after all. Such difficulties with decisions crop up in all aspects of life, not only food. However, they predominantly affect preference-based decisions, i.e. questions like «what do I prefer - melon or cherries?" Purely sensory decisions based on sensorial information such as «what is bigger - melon or cherry?" are less prone to indecisiveness.
The more intensive the information flow, the more decisive
How come some people are so uncertain of their preferences and keep making new choices while others know exactly what they like and want? A team headed by Professor Christian Ruff, a neuroeconomist from the University of Zurich, set about investigating this question. The Zurich researchers discovered that the precision and stability of preference decisions do not only depend on the strength of the activation of one or more brain regions. Instead, the key for stable preference choices is the intensity of the communication between two areas of the brain which represent our preferences or are involved in spatial orientation and action planning.
The researchers used transcranial alternating current stimulation, a non-invasive brain stimulation method that enables generation of coordinated oscillations in the activity of particular brain regions. The test subjects did not realize that they were being stimulated. Using this technique, the researchers intensified or reduced the information flow between the prefrontal cortex located directly below the forehead and the parietal cortex just above both ears. The test subjects had to make preference-based or purely sensory decisions about food.
«We discovered that preference-based decisions were less stable if the information flow between the two brain regions was disrupted. Our test subjects were therefore more indecisive. For the purely sensory decisions, however, there was no such effect," explains Ruff. «Consequently, thecommunication between the two brain regions is only relevant if we have to decide whether we like something and not when we make decisions based on objective facts." There was no evidence of any gender-specific effects in the experiments.
It was not possible to make the decisions more stable by intensifying the information flow. However, the study participants were young, healthy test subjects with highly developed decision-making skills. On the other hand, the results of the study could be used for therapeutic measures in the future - such as in patients who suffer from a high degree of impulsiveness and indecisiveness in the aftermath of brain disorders.
Read the original article Here
- Comments (0)
- Brain Scans Predict Success of CBT for Social Anxiety Disorder
- By Jason von Stietz
- August 20, 2015
-
.jpg)
Photo Credit: MIT News Social anxiety disorder (SAD) affects 15 million people in the United States, approximately 6.8 percent of the U.S. population. Unfortunately, many treatments of SAD succeed as often as they fail. However, researchers at MIT found that brain scans predicted which patients would benefit from CBT with an accuracy of 80 percent. Medical Xpress discussed the findings in a recent article:
For patients with social anxiety disorder (SAD), current behavioral and pharmaceutical treatments work about half the time. After weeks of investment in therapy, about half of patients will likely still suffer with symptoms of anxiety, and have little choice but to try again with something else. This trial-and-error process—inevitable due to an absence of tools to guide treatment selection—is time-consuming and expensive, and some patients eventually just give up.
But new MIT research suggests that it may be possible to do better than a coin toss when choosing psychiatric therapies for patients. The study, which performed brain scans on 38 SAD patients, found that these scans contain clues that indicate, with about 80 percent accuracy, which SAD patients will do well in cognitive behavioral therapy (CBT), an intervention designed to help patients change thinking patterns. Use of the scans to predict treatment outcomes improved predictions fivefold over use of a clinician's assessment alone.
"Choice of therapy is like a wheel of chance," says first author Susan Whitfield-Gabrieli, a research scientist in the McGovern Institute for Brain Research at MIT. "We're hoping to use brain imaging to help provide more reliable predictors of treatment response."
The researchers used a form of brain imaging that scans patients in a state of rest. Resting-state images can be done quickly, in about 15 minutes, and reliably, since they don't require patients to follow instructions, so they have the potential to be used in a clinical setting as a tool that helps doctors select the best treatments for patients.
"Knowing who to give which therapy to upfront would save time, money, and health care resources," says Greg Siegle, an associate professor of psychiatry at the University of Pittsburgh School of Medicine who was not involved in this study. "This ability would be staggering to have at our disposal for the health care system."
The findings are reported in the current issue of the journal Molecular Psychiatry. The work was carried out in the lab of principal investigator John Gabrieli, the Grover Hermann Professor of Health Sciences and Cognitive Neuroscience at MIT and a member of the McGovern Institute.
Common disorder
Social anxiety disorder affects approximately 6.8 percent of Americans, about 15 million individuals, and is the country's third-most-common mental health disorder, according to the National Institutes of Mental Health. Its symptoms include extreme anxiety in social settings that can interfere with work and quality of life. Patients living with this disorder are also at higher risk of other psychiatric disorders, such as depression and substance abuse.
The study analyzed SAD patients from the Center for Anxiety and Related Disorders at Boston University and the Center for Anxiety and Traumatic Stress at Massachusetts General Hospital. The patients were scanned prior to participation in 12 weeks of group-based CBT. They also were evaluated using a behavioral assessment tool called the Liebowitz Social Anxiety Scale (LSAS) before and after CBT to determine who had improved.
In 2013, co-author Satrajit Ghosh, a principal research scientist at the McGovern Institute, studied task-based scans of this same group of patients. He and Whitfield-Gabrieli found that scans of patients' brains as they responded to angry or neutral faces and emotional or neutral scenes predicted CBT outcomes.
"But task-based scans have downsides," Whitfield-Gabrieli says: Behavioral differences among patients can affect performance. Also, task-based scans can only be used on patients who can follow a task, which excludes infants and some elderly or very ill patients.
Scanning the resting brain
So Whitfield-Gabrieli followed this earlier research with a study of the predictive power of resting-state imaging, which she and colleagues had also performed prior to CBT. During a resting-state scan, the patient just lies there. "That's the beauty of it," she says. "They're just letting their minds wander."
Resting-state imaging provides a look at the way a patient's brain is wired, both structurally and functionally. For instance, resting-state functional magnetic resonance imaging (fMRI) shows which parts of the brain synchronize with one another during rest, suggesting that they are functionally connected. In addition, analysis of diffusion-weighted magnetic resonance imaging (dMRI) shows the underlying anatomy of the white matter tracts that interconnect distant brain regions.
Based on findings from their earlier research, Whitfield-Gabrieli and colleagues first used resting-state fMRI to look at connections to the amygdala, the seat of fear in the brain. They found that patients with higher connectivity to the amygdala from certain other regions were more likely to have lower anxiety after CBT.
They then performed a second analysis of the resting-state fMRI data, this time looking across the entire brain for patterns of connectivity. This analysis revealed additional markers that were predictive of treatment. The researchers also analyzed dMRI data and found that more robust connectivity in the tract that connects visual cues with emotional responses is also predictive of improvement with CBT.
Higher LSAS scores, which indicate more severe SAD, correlate modestly with larger improvements after CBT. In this study, each brain scan analysis had predictive value beyond the LSAS, and the three analyses together produced a fivefold improvement in predictive power over the LSAS alone.
The next step for Whitfield-Gabrieli and colleagues is to validate their predictive model on hundreds or possibly thousands of patients. Such a large-scale study may be possible because resting-state scans are comparable even when performed in different labs or by different researchers. Such comparisons weren't feasible using task-based scans, which tend to vary from lab to lab.
"Right now there's a huge movement to create massive data sets, to share resting-state imaging data, and really change the way people do science," Whitfield-Gabrieli says.
Other next steps for Whitfield-Gabrieli's group are studies to predict the success of more than one form of therapy, and to look at other psychiatric conditions, such as depression and attention disorders. "We don't want to just know if they're going to respond to one treatment," she says. "We want to know which treatment is best for each patient."
Read the original article Here
- Comments (0)
- Electrical Signals Might Facilitate the Repair of Spinal Cord Injuries
- By Jason von Stietz
- August 7, 2015
-
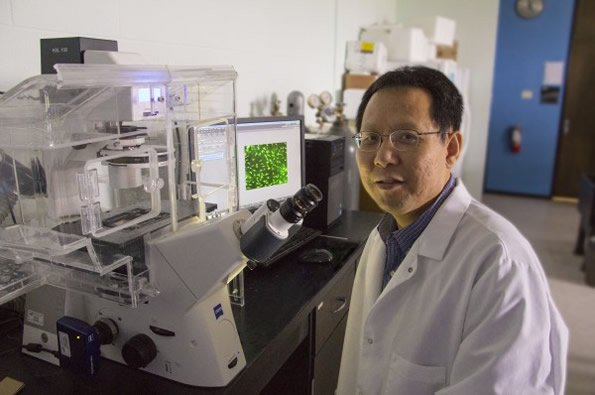
Researcher Li Yao. Photo Credit: Wichita State University Can the spinal cord heal itself after an injury? A researcher at Wichita State University is investigating a promising new approach that involves aiming electrical signals at the spinal cord that facilitate healing. A recent article in NeuroScientistNews discusses the new approach:
Wichita State University's Li Yao is taking a special approach to the study of spinal cord injuries through research that uses an electrical signal to repair tissue damage.
When a person suffers neurological damage to their spinal cord, the tissues surrounding the injury site can die. But one of the body's defense mechanisms is the regeneration and migration of a type of support cell -- called Schwann cells -- to the injury.
Those cells, as has been discovered in recent years, help myelinate -- or cover -- nerve axons where the injury has occurred, which promotes the recovery of some of the spinal cord's function.
Yao, a biological sciences assistant professor, is studying how electrical signals can aim those cells directly to the injury site. His research, he hopes, will open new doors for the medical field to use electrical fields in the treatment of neural injuries.
"Electrical signal is a kind of ignored approach that may generate significant biological function in neural regeneration," Yao says.
Yao's research studies the molecular mechanism of cell migration in electric fields using next-generation RNA sequencing to look at the signaling pathways that regulate cell migration.
So far, he has discovered that the precision of the cell migration toward the injury increased significantly as the strength of the electrical field increased. The electrical field did not, however, change the speed at which the cells moved.
Still, Yao's early findings suggest that the use of electrical fields in cell migration could become a burgeoning area of study in regenerative medicine.
"Our work has implications for central nervous system repair, and the application of an electrical field may assist with that," Yao says.
Read the original article Here
- Comments (0)
- Transcranial Magnetic Stimulation: A Non-Drug Treatment Option for Depression
- By Jason von Stietz
- July 29, 2015
-

Photo Credit: Getty Images It is estimated that 7 percent of people in the United States live with clinical depression. Transcranial magnetic stimulation (TMS), involves stimulating the prefrontal cortex, which is found to be under-activated in people with depression. TMS is a non-drug treatment option that is beginning to find favor among clinicians and researchers, alike. A recent article in the Tribune discussed the empirical research and the experience of clinicians supporting TMS:
Depression lifted from Nick O'Madden's life like a set of foggy glasses being wiped clean.
Earlier this summer, O'Madden, 31, felt he was living in a distracted haze, sprinkled with nighttime panic attacks. Now, after undergoing an emerging high-tech treatment involving magnetic currents, he said he's literally seeing the world in a new light.
"Colors are brighter," said O'Madden, a mental health therapist who lives in Elk Grove, Calif. "Last night, I was looking at the moon, and it just looked clearer and brighter and more beautiful ... It's almost kind of scary to see that at first, it's so new to me."
He described the changes from a reclined medical chair at TMS Health Solutions, a treatment center in Sacramento's Campus Commons area that specializes in transcranial magnetic stimulation. With a metal coil positioned near his forehead, he spoke between bouts of jackhammer-esque pulsing that erupted every 15 seconds during the 50-minute session.
The "train pulses," as technicians call the strings of sound, are actually the back-and-forth flexing of the metal coil as the device sends out a 2-tesla-strong magnetic current. The coil creates a magnetic field that reaches 2 to 3 centimeters into brain matter to stimulate the dorsal-lateral prefrontal cortex, the poker chip-sized area responsible for regulating mood, memory and decision-making.
An estimated 7 percent of American adults suffer from clinical depression, which can cause lethargy, indifference, moodiness and other symptoms that interfere with day-to-day functioning. Researchers have found that the prefrontal cortex is often underactive in people diagnosed with the illness.
The TMS technology uses electric currents to excite cell activity in that part of the brain, theoretically helping neurons better communicate with one another and increasing blood flow to the tissue, which promotes healthy brain function. The federal Food and Drug Administration has approved the treatment, but for limited use given that it is relatively new. Physicians can administer it only to patients who haven't responded to at least one prescription medication for depression.
Advocates of the treatment refer to it as revolutionary; there hasn't been a major development in procedure-based depression treatment since the advent of electroconvulsive therapy. Unlike that treatment, which applies electricity directly to the skull to invoke a brain seizure, the magnetic TMS procedure has not shown negative impact on memory or cognition.
TMS, and other new treatments that focus on physical stimulation of specific parts of the brain, signal a departure from traditional methods of treating mental illness, such as talk therapy and prescription drugs. As advances in medical technology allow researchers to better understand how the human brain functions, approaches to treatment are following suit.
"There's a growing recognition, both with scientists and patients, that depression is a brain problem - a problem with chemicals in our circuitry," said Dr. Paul Croarkin, a psychiatrist with the Mayo Clinic. "The fact that we're soon going to have more and more offerings in that regard is a positive thing."
As with many emerging medical treatments, practitioners and insurers hesitate to embrace new procedures without a solid track record. Though the FDA approved the nation's first TMS device in 2008, major health insurance companies have only begun covering the treatment in the past few years.
Dr. Richard Bermudes is principal owner and medical director of TMS Health Solutions and president of the nationwide Clinical TMS Society. By his estimate, about 700 TMS devices are in use in the United States.
The treatment has been the focus of about 30 randomized clinical trials in the United States, and in most of those, a statistically significant portion of patients were determined to have benefited. But some researchers caution that the improvements could be the result of a placebo effect, and have called for longer-term studies.
A 2012 study published in the Journal of Clinical Psychiatry showed that half of the patients involved in that trial responded to the treatment within six weeks, and 25 percent went into remission. Still, guidelines from the Agency for Healthcare Research and Quality and the Department of Health and Human Services state that evidence is "insufficient to evaluate the ability of (repetitive) TMS to maintain response or remission."
On the upside, the therapy has not been shown to cause whole-body side effects, such as weight gain or fatigue, as an oral medication might, said Dr. Guohua Xia, a clinical associate professor at University of California-Davis and medical director of Brainefit, a mental health institute offering a form of TMS services. That means it can be especially helpful for pregnant women and elderly people who may experience problems with standard depression drugs.
Sutter Health is the only hospital system in Sacramento to offer the treatment. Dr. Theodore Goodman, director of interventional psychiatry for Sutter Health, said TMS has resulted in improvement for about 60 percent of patients during the two years it has been offered at the Sutter Center for Psychiatry.
He expressed frustration at insurance companies not covering the treatment long term. TMS is currently approved only as a treatment for acute clinical depression, meaning patients are in the throes of symptoms.
"About 50 percent of patients will relapse over a year's time," he said. "The way you avoid that is maintenance treatment, but insurance won't pay for that. It's a horribly unenlightened viewpoint."
While NeuroStar, the model used at Bermudes' clinic, was the first TMS device approved on the market, other brands go even further into brain matter and have been used to target other conditions, including migraines.
At TMS Health Solutions, the recommended treatment plan is four to six weeks of daily TMS sessions, at a cost of $5,000 to $7,000. Since opening clinics in El Dorado Hills, Calif., in 2007 and Sacramento in 2010, Bermudes said, he has used the technology to treat hundreds of patients and currently sees about 20 TMS patients a day.
He said he recently changed the clinic's name - from Mindful Health Solutions - specifically to highlight the treatment.
"There's not a lot of access to this modality currently in the community," he said. "A lot of our patients have been depressed for years before coming to TMS. If we can get people into TMS earlier, our remission and response rates may go up."
O'Madden said that, for him, improvement came after three weeks of treatment, though technicians say results can take longer. Before his physician suggested TMS, O'Madden said, he was having trouble sleeping and focusing, and struggled to control anxiety and obsessive thought patterns.
He said he's now feeling more focused and active, with a renewed passion for boxing. He recently started a blog to document his recovery.
"I want people to become more aware of (TMS), and I also want mental health to be less stigmatized," he said. "I want people to see me as a person: I'm a father and a husband, but I suffer from a mental health disorder, and I'm seeking help ... and other people can do the same thing."
Read the original article Here. For additional information about TMS visit Brain Wellness Center. Brain Wellness Center is located in San Ramon and Palo Alto and is one of the leading edge providers of TMS services. Each patient’s qEEG brain mapping information is utilized to customize and tailor make the treatment to their specific and unique brain pattern.
- Comments (8)
- Brain Circuit Involved in Inheritance of Anxiety in Rhesus Monkeys
- By Jason von Stietz
- July 17, 2015
-

Photo Credit: Getty Images Anxious parents are likely to have anxious children. This is true of rhesus monkeys as well as humans. Researchers at the University of Wisconsin, Madison utilized positron emission topography (PET) scans to study anxiety in multiple generations of rhesus monkeys. Findings indicated that the inheritance of an over-active brain circuit might set the stage for the development of anxiety or depressive disorders. The study was discussed in a recent issue of NeuroScientistNews:
In rhesus monkey families -- just as in their human cousins -- anxious parents are more likely to have anxious offspring. And a new study in an extended family of monkeys provides important insights into how the risk of developing anxiety and depression is passed from parents to children.
The study from the Department of Psychiatry and the Health Emotions Research Institute at the University of Wisconsin-Madison shows how an over-active brain circuit involving three brain areas inherited from generation to generation may set the stage for developing anxiety and depressive disorders.
The study is published online in the early edition of the Proceedings of the National Academy of Sciences. It shows that elevated activity in this prefrontal- limbic -midbrain circuit is likely involved in mediating the in-born risk for extreme anxiety, anxious temperament that can be observed in early childhood.
"Over-activity of these three brain regions are inherited brain alterations that are directly linked to the later life risk to develop anxiety and depression,'' says senior author Dr. Ned Kalin, chair of psychiatry at the UW School of Medicine and Public Health. "This is a big step in understanding the neural underpinnings of inherited anxiety and begins to give us more selective targets for treatment."
Previous research by Kalin's group has shown that anxious temperament is inherited, and explained the brain circuits involved. About half of children who show extreme anxiety go on to develop stress-related psychiatric disorders later in life.
Monkeys, like humans, can be temperamentally anxious and pass their anxiety-related genes on to the next generation.
By studying nearly 600 young rhesus monkeys from a large multi-generational family, Drs. Andrew Fox, Kalin, and colleagues found that about 35 percent of variation in anxiety-like tendencies is explained by family history.
To understand which brain regions are responsible for passing anxiety from generation to generation, the authors measured anxiety-related behavior with high-resolution functional and structural brain imaging. They exposed the young monkeys to a mildly threatening situation that a child would also encounter, exposure to a stranger who does not make eye contact with the monkey. During this encounter, they used imaging methods commonly used in humans (positron emission tomography, PET) to identify brain regions in which increased metabolism predicted each individual's level of anxiety.
By closely examining how individual differences in brain function and anxiety-related behavior fall through the family tree, the authors identified brain systems responsible for the parent-to-child transmission of anxiety-related behavior. Using this "genetic correlation" approach, the authors found the neural circuit where metabolism and an early-life anxious temperament are likely to share the same genetic basis.
Interestingly, the brain circuit that was genetically correlated with individual differences in early-life anxiety involved three survival-related brain regions. These regions were located in the brain stem, the most primitive part of the brain; the amygdala, the limbic brain fear center; and the prefrontal cortex, which is responsible for higher-level reasoning and is fully developed only in humans and their primate cousins.
"Basically, we think that to a certain extent, anxiety can provide an evolutionary advantage because it helps an individual recognize and avoid danger, but when the circuits are over-active, it becomes a problem and can result in anxiety and depressive disorders," Kalin explains.
Surprisingly, these studies found that it was the function of these brain structures -- and not their size -- that was responsible for the genetic transfer of an anxious temperament. Although the search for the genetic underpinnings of anxiety have thus far been elusive, this research helps explain how genes might affect brain function and lead to extreme childhood anxiety, which greatly increases the risk to develop anxiety and depressive disorders.
"Now that we know where to look, we can develop a better understanding of the molecular alterations that give rise to anxiety-related brain function,'' Kalin says. "Our genes shape our brains to help make us who we are."
Read the original article Here
- Comments (0)
- Animal Study Sheds Light on Neurocircuitry Involved in Resiliency
- By Jason von Stietz
- July 10, 2015
-

Getty Images Why are some resilient to chronic stress and not others. Findings from a recent animal study of chronic social defeat stress sheds light on the neurocircuitry involved in vulnerability or resiliency to stress. NeuroScientistNews discussed the study in a recent article:
Humans are remarkably resilient when confronted with tremendous amounts of stress and trauma. While most people are able to maintain balanced psychological and physical functioning, some people are vulnerable, or susceptible, to the negative biological, psychological, and social consequences of stress. The biological factors underlying susceptibility are unknown and likely intersect with an individual’s ability to cope, among other factors.
Emerging evidence from animal studies suggests there are distinct cellular and molecular adaptations that occur in response to stress to either promote resiliency or lead to susceptibility. The ventral striatum (vSTR) has been identified as a key brain region for regulating depression-related behaviors following chronic stress. In a recent study, Christoffel et al. elucidated the specific inputs to the vSTR mediating susceptibility to stress in mice following chronic social defeat stress (CSDS). CSDS is a well-validated model for studying the cellular and molecular underpinnings of stress-related psychiatric diseases in rodents.
The CSDS paradigm consists of pairing an experimental C57BL/6J mouse with an aggressive, CD-1 retired breeder mouse over the course of days in a cage. After each daily pairing, these mice are housed in the same cage, only separated by a partition with holes to allow for continuous ‘psychological’ stress for the experimental mouse from sensory interaction with the aggressor mouse. Following CSDS, the experimental mice are tested in the social interaction behavioral assay to assess the degree of social avoidance (i.e., anxiety and depression related behavior). The experimental mouse is placed into an open arena with the caged aggressor mouse and the amount of time spent socially interacting is recorded. Despite experiencing the same defeat stressor, experimental mice can be separated into ‘susceptible’ or ‘resilient’ groups to study the biological mechanisms contributing to these divergent phenotypes.
The authors used complementary approaches to identify and manipulate specific excitatory, glutamatergic inputs to the vSTR that mediate stress susceptibility. Projection-based viral targeting techniques revealed increased excitatory synaptic strength from the intralaminar (ILT) to the vSTR only in susceptible mice, whereas excitatory strength of the inputs to the vSTR from the prefrontal cortex (PFC) was similar between resilient and susceptible mice, suggesting enhanced ILT-vSTR signaling is relevant for stress-induced susceptibility.
Interestingly, inhibition of the ILT presynaptic inputs to the vSTR either by chronically inhibiting calcium release using viral-mediated expression of ‘tToxins’ or acutely by physiologically relevant optogenetic inhibition prevented stress-induced susceptibility, which was accompanied by reductions in excitatory postsynaptic currents (EPSCs) and the density of immature stubby dendritic spines of vSTR medium spiny neurons (MSNs).
In contrast, chronic inhibition of PFC-vSTR pathways further decreased stress-induced social interaction times and increased the density of stubby dendritic spines in the vSTR. However, acute, rapid optogenetic inhibition of this circuit had no effect on the susceptibility phenotype, suggesting sustained inhibition may be required, or other PFC efferents are responsible for promoting normal behavioral function (i.e., resiliency).
Human imaging findings indicate reduced vSTR response to various rewarding stimuli in individuals with major depressive disorder1,2,3, which are further supported by studies using deep brain stimulation of the internal capsule (includes vSTR) to alleviate symptoms of depression4. The present findings suggest that distinct glutamatergic pathways converge on the vSTR reward circuitry to mediate stress-induced susceptibility or promote resiliency. Animal studies are beginning to shed light on how stress leads to alterations in activity of particular neural circuits that could be relevant for many psychiatric diseases.
Read the orginal article Here
- Comments (0)
- Hippocampus Smaller in People with Recurrent Depression
- By Jason von Stietz
- July 3, 2015
-
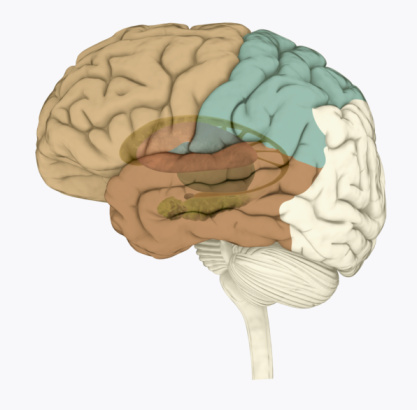
Photo Credit: Getty Images Recent research has found that the hippocampus of people with recurrent depression is significantly smaller than that of healthy individuals. Researchers from the University of Sydney examined the magnetic resonance imaging (MRI) data of nearly 9,000 participants. The findings were recently discussed in an article of Medical Xpress:
Major depression is a common condition affecting at least one in six people during their lifetime. It is a serious clinical mood disorder in which feelings of sadness, frustration, loss, or anger interfere with a person's everyday life for weeks, months or years at a time.
Key findings
The key finding that people with major depression have a smaller hippocampus confirms earlier clinical work conducted at the BMRI. In this study, the key finding was largely explained by subjects with recurrent depression. People with recurrent depression represented 65 per cent of study subjects with major depression.
People with an early age of onset of major depression (before the age of 21 years) also had a smaller hippocampus than healthy individuals, consistent with the notion that many of these young people go on to have recurrent disorders.
However, people who had a first episode of major depression (34 per cent of study subjects with major depression) did not have a smaller hippocampus than healthy individuals, indicating that the changes are due to the adverse effects of depressive illness on the brain.
Commentary
"These findings shed new light on brain structures and possible mechanisms responsible for depression," says Associate Professor Jim Lagopoulos of the University of Sydney's Brain and Mind Research Institute.
"Despite intensive research aimed at identifying brain structures linked to depression in recent decades, our understanding of what causes depression is still rudimentary.
"One reason for this has been the lack of sufficiently large studies, variability in the disease and treatments provided, and the complex interactions between clinical characteristics and brain structure."
Commenting on the clinical significance of the findings, Co-Director of the Brain and Mind Research Institute, Professor Ian Hickie says: "This large study confirms the need to treat first episodes of depression effectively, particularly in teenagers and young adults, to prevent the brain changes that accompany recurrent depression.
"This is another reason that we need to ensure that young people receive effective treatments for depression - a key goal of our Centre of Research Excellence in Optimising Early Interventions for Young People with Emerging Mood Disorder. "This new finding of smaller hippocampal volume in people with major depression may offer some support to the neurotrophic hypothesis of depression," adds Jim Lagopoulos.
"This hypothesis argues that a range of neurobiological processes such as elevated glucocorticoid levels in those with chronic depression may induce brain shrinkage.
"Clearly, there's a need for longitudinal studies that can track changes in hippocampal volume among people with depression over time, to better clarify whether hippocampal abnormalities result from prolonged duration of chronic stress, or represent a vulnerability factor for depression, or both," he said.
Read the original article Here
- Comments (0)


 Subscribe to our Feed via RSS
Subscribe to our Feed via RSS